Past Conference 2024
2024 CMS Quality Conference
 April 8, 2024 09:00
April 8, 2024 09:00How to Begin a Medicaid and Chip Quality Improvement Project: Skills, Stories, and Resources

Deirdra Stockmann, PhD, MUP, (Moderator)
Director,
Division of Quality and Health Outcomes,
Center for Medicaid and
CHIP Services,
Centers for Medicare & Medicaid Services

Jane Taylor, MHA, MBA, ED.D.
Improvement
Advisor,
Jane A. Taylor, ED.D., LLC

Tony Richards, MPH, PMD Pro
Director,
Office of
Child Welfare,
Center for Managed Care,
Bureau for Medical Services,
West Virginia
Department of Health and Human Resources
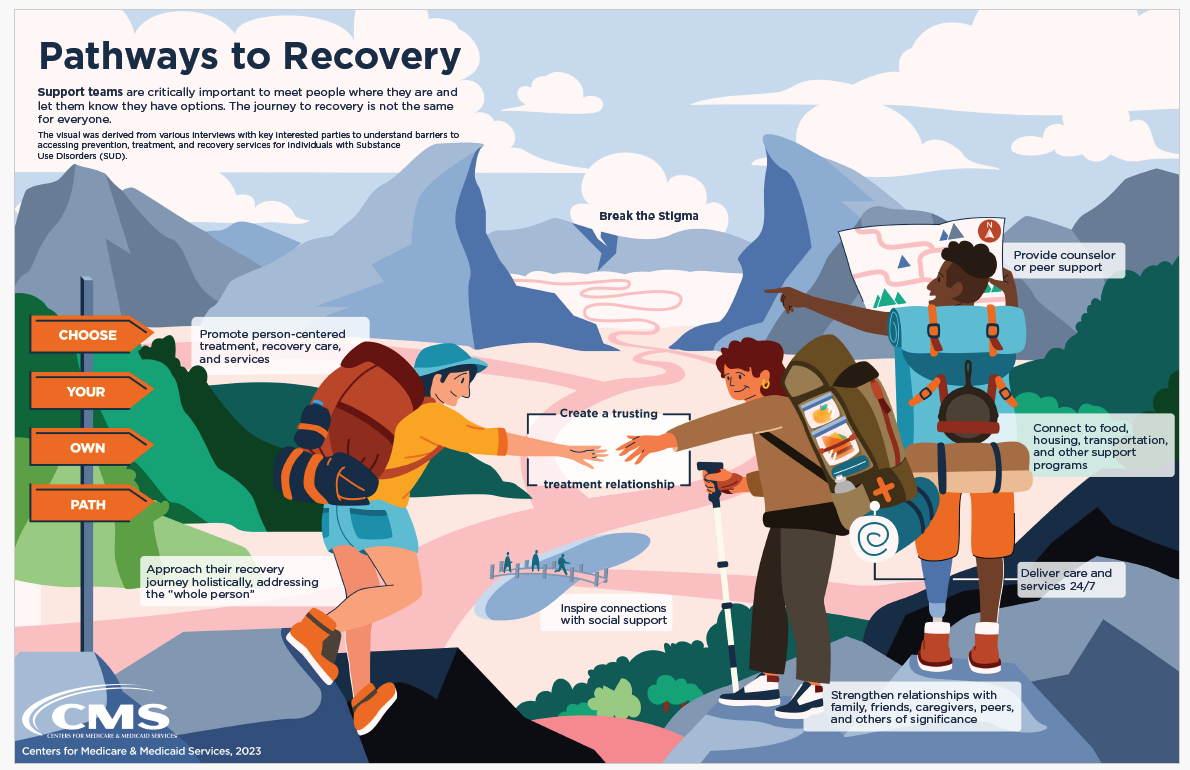
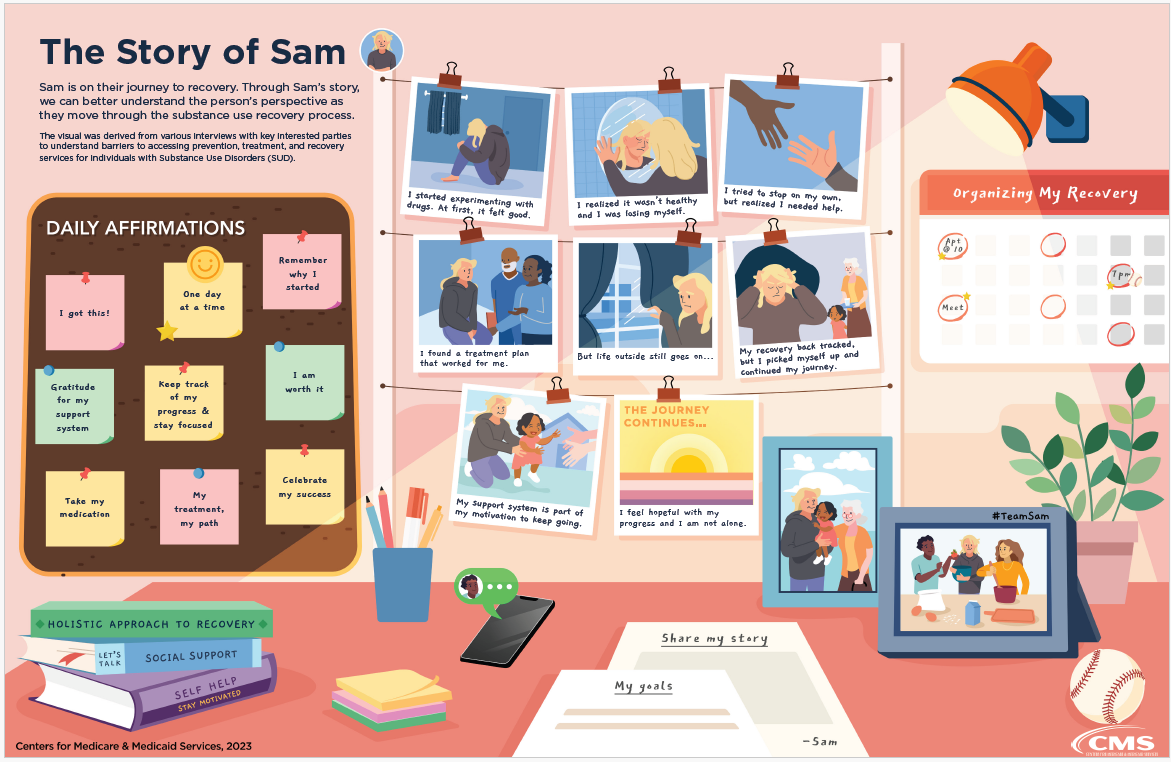
Effective quality improvement (QI) begins by understanding the problem you are trying to solve. This mini plenary will discuss several tools that Medicaid and Children's Health Insurance Program (CHIP) agency staff can use to understand challenges and identify solutions for QI, as well as help identify the measures and partners needed to effect change. Participants will hear from an improvement advisor and state speaker who will describe these tools and how they applied them in their QI efforts. The class will also review new resources and tools developed by CMS to help state staff and their QI partners address other key areas of improvement in Medicaid and CHIP programs.
 April 8, 2024 09:00
April 8, 2024 09:00Building a Climate-resilient, Sustainable Health System in Service of the Most Vulnerable Beneficiaries

Anita Monteiro
Director, iQuality
Improvement &
Innovation Group
Centers for Medicare & Medicaid Services

Joe McCannon
Special Expert and
Senior Advisor,
Agency for Healthcare Research and Quality/Office of Climate Change and
Health Equity
Climate change represents an unprecedented threat to the health of people around the world, particularly certain groups that – for reasons of long-time discrimination, disenfranchisement, and underinvestment – are much more exposed to climate-related harm. Given this, the Biden Administration created a new Office of Climate Change and Health Equity (OCCHE) to mobilize all of HHS to act in support of communities and providers across the country addressing this challenge. In this session, the OCCHE team and colleagues from CMS will describe the scope and nature of climate-related threats to health, and tools and resources to support providers and other stakeholders in tackling them, including billions of dollars in tax credits and grants from the Inflation Reduction Act and forthcoming programming from CMS.
 April 8, 2024 09:00
April 8, 2024 09:00Enhancing Workforce Resilience & Well-Being: Rediscovering Joy in Health Care

Lotte Dyrbye, MD, MHPE
Senior
Associate Dean of
Faculty and Chief Well-being Officer,
University of Colorado School of
Medicine
Lee Daugherty Biddison, MD, MPH
Chief Wellness
Officer,
Director of Credentialing,
Associate Professor,
Johns
Hopkins School of
Medicine

Christine Sinsky, MD
Vice
President of Professional
Satisfaction,
American Medical Association
CMS is committed to promoting clinician well-being through our efforts to support clinicians and systems in providing high quality care, and to identify and reduce administrative burden. A systems approach to promoting well-being and resilience in health care is a cornerstone of the National Academy of Medicine’s Action Collaborative on Clinician Well-Being and Resilience. This session will explore insights and tools from four leaders in this field who are working to strengthen and energize the health care workforce by better understanding the factors that lead to clinician burnout and promoting joy in health care. Speakers from the American Medical Association (AMA), the University of Colorado School of Medicine, Duke University Health System and Johns Hopkins Medicine will discuss the negative impact of health care worker burnout on both individuals and health care systems, and share strategies organizations can use to support well-being and resilience and create space for health care workers to stay energized and deliver excellent care.
Click Here to View Presentation
 April 8, 2024 10:30
April 8, 2024 10:30Welcome

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services
 April 8, 2024 14:00
April 8, 2024 14:00Guiding Dementia Care Decisions: What Matters

Adrienne Mims, MD, MPH, AGSF
Chief Medical
Officer,
Rainmakers Strategic Solutions

Shari Ling, MD (Moderator)
Deputy CMS Chief
Medical Officer,
Centers for Medicare & Medicaid Services
Esther Oh, MD, PhD
Associate
Professor of
Medicine,
Psychiatry and Behavioral Sciences and Pathology,
Johns
Hopkins University School
of Medicine

Tonya Saffer, MPH
Director,
Division of
Healthcare Payment Models within the Patient Care Models Group,
Center
for Medicaid and CHIP
Services,
Centers for Medicare & Medicaid Services
This is In Person Session.
Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD) affect as many as six million people in the United States, a number expected to more than double by 2060. AD/ADRD are debilitating conditions that impair memory, thought processes, and function, primarily among older adults. The chance of developing dementia is not equal—Black and Latino Americans are more likely to develop AD/ADRD, as are people with risk factors such as high blood pressure, diabetes, and depression.
AD/ADRD has physical, psychological, social, and economic impacts for the person, families and caregivers, communities, and the nation. Person-centered care is effective for people living with dementia when care goals are known and used to guide nonpharmacologic and pharmacological treatment. This session will address the importance of person-centered, patient-clinician decision making and identify ways to use the approach in dementia care planning broadly.
 April 8, 2024 14:00
April 8, 2024 14:00Addressing Substance Use Disorder and Serious Mental Illness Through Medicaid and CHIP Demonstrations

Sarah Sheets, MPhil
Research
Analyst,
State
Demonstrations Group,
Center for Medicaid and CHIP Services,
Centers
for Medicare and
Medicaid Services

Leslie Hoffman, M.Ed., LSSYB
Kentucky Cabinet for
Health and Family Services,
Department for Medicaid Services

Danielle Daly, PhD, MS
State
Demonstrations
Group,
Center for Medicaid and CHIP Services,
Centers for Medicare
and Medicaid
Services

Angela Sparrow, MSW, CSW
Behavioral Health
Supervisor,
Kentucky Cabinet for Health and Family
Services,
Department for Medicaid
Services
This is In Person Session
This session will explore findings from section 1115 Substance Use Disorder (SUD; (#17-003 RE: Strategies to Address the Opioid Epidemic) and Serious Mental Illness (SMI; #18-011 Opportunities to Design Innovative Service Delivery Systems for Adults with a Serious Mental Illness or Children with a Serious Emotional Disturbance) demonstrations. States conduct structured monitoring and rigorous evaluations of the demonstrations, and the Centers for Medicaid and CHIP Services (CMCS) conducts federal monitoring and evaluation of both demonstration opportunities to support identifying best practices and learning and diffusion. CMCS will share key findings and discuss how it uses findings. Based on data submitted to CMS through June 2022, between the baseline and Demonstration Year 3 and later, the demonstrations were associated with a 17.1 percent increase in the number of beneficiaries using SUD treatment services. For beneficiaries with opioid use disorder (OUD), the demonstrations were associated with an increase in the share of beneficiaries receiving medication assisted treatment (MAT). However, overdose death rates increased in 10 out of 14 states and the rate of ambulatory/preventive care use declined in 11 of 14 states. Presenters will discuss state activities to address findings, including but not limited to strategies to increase access to MAT. Lastly, Kentucky will share how their team uses the information to inform continuous process and quality improvement of the demonstration.
 April 8, 2024 14:00
April 8, 2024 14:00Telehealth: Improving Access to Care for Tribes: CMS and IHS Updates

Susan Karol, MD
Chief Medical
Officer,
Division
of Tribal Affairs,
Centers for Medicare & Medicaid Services

Susy Postal, DNP, RN-BC
Chief
Informatics
Officer,
Indian Health Service
Chris Fore, PhD
Director,
Indian Health
Service Telebehavioral Health Center of Excellence
This is In Person Session
The Indian Health Service (IHS) continues to support the expanded use of telehealth to provide patient care after the COVID-19 Public Health Emergency (PHE). This presentation will focus on an overview of the use of telehealth at the IHS and the support the Centers for Medicare & Medicaid Services (Centers for Medicare & Medicaid Services) provides. The presentation will include the accomplishments in expanding telehealth from April 2020 to the present. The various telehealth services available at the IHS will be discussed including Centers for Medicare & Medicaid Services’ support provided to rural and frontier areas. Issues in providing audio-only services will be discussed and aligned with services on the Medicare Telehealth Services List for CY 2024. Presenters will provide metrics describing the utilization of telehealth in IHS. Telehealth best practices will be discussed, and quantitative and qualitative results from IHS patient and IHS provider telehealth surveys will be addressed. Finally, patient outcomes utilizing telehealth services will be included and quality improvement options provided.
 April 8, 2024 14:00
April 8, 2024 14:00Innovation Center Quality Pathway – A Refreshed Approach to Quality in CMMI Models
Noemi Rudolph, MPH
Director,
Research and Rapid
Cycle Evaluation Group,
Center for Medicare and Medicaid Innovation
(CMMI)

Jacob Quinton, MD, MPH
Medical
Officer,
Center
for Medicare and Medicaid Innovation (CMMI),
Centers for Medicare &
Medicaid
Services

Susannah Bernheim, MD, MHS
Chief
Quality Officer
& Acting Chief Medical Officer,
Center for Medicare and Medicaid
Innovation,
Centers
for Medicare & Medicaid Services
This is In Person Session
The purpose of the proposed panel is to describe the CMS Innovation Center’s approach to strengthening the focus on quality, outcomes, and experience within the Innovation Center’s alternative payment models. The resulting Quality Pathway emerged from the 2021 strategic refresh and includes development of a process to certify models for expansion based on quality improvement. The panel will introduce the pathway, describing how it elevates patient outcomes and experience of care within alternative payment models and emphasizes the translation of a model’s theory of action into measurable benefits for patients. The panel will discuss how this alignment of model design and quality strategy also drives new approaches to model evaluation, and how the Quality Pathway will be used to identify when a model may be eligible for expansion based on demonstrated quality improvement in alignment with CMMI’s statutory mandate. Having addressed the conceptual basis for the Pathway, the panel will share examples of models recently under development to demonstrate how the pathway will be used at the Center. This will include insight into design choices around measure selection, implementation decisions on data collection, and evaluation considerations on methodological approach. As part of discussing implementation of the pathway, the panel will identify a number of considerations entailed in executing this new approach to model quality strategies at the Center, such as those associated with novel measure development and rigorously evaluating the impact of models on patient outcome and experience.
 April 8, 2024 14:00
April 8, 2024 14:00Top of the List: Ensuring Transplant Readiness in Those Likely to Soon Receive an Organ Offer

Mercedes Islas, BSN, RN
Froedtert
Memorial Lutheran
Hospital
Michael Mace, MSW, LICSW
Nephrology Social
Worker,
Fresenius Kidney Care
Assuring the transplantation of every kidney offer includes ensuring that those patients who are likely to soon receive an organ offer are prepared to accept. Froedtert Memorial Lutheran Hospital’s quality improvement activities highlighted a potential opportunity for refinement in this aspect of the pre-transplant process. Beginning in Spring 2023, the transplant team developed and executed an enhanced patient preparation called Top of the List to meet this need.
From the perspective of a long-time dialysis social worker and transplant recipient, Mr. Mace will bring his insights on supporting patients waiting for a transplant. He will also share his experience on how to build collaborative communication and standard processes between the dialysis facility and the transplant program to ensure patients are transplant ready.
Top of the List focuses on ensuring patients based upon the OPTN allocation sequence at the top of each blood type are “transplant ready.” Froedtert’s enhancements to the process included: weekly calls to the patient from the pre-transplant coordinator, immediate review of medical records including updates from dialysis units, weekly care team meetings with multi-disciplinary review, and weekly emails to the patients’ dialysis centers to ensure timely communication on pertinent patient issues or changes in status. While outcome data is still being collected, the process shows potential to increase organ offer acceptance and simplifying activities when the offer is made.
 April 8, 2024 14:00
April 8, 2024 14:00Home Therapy Innovation Through Culture Change

Tammy Carmean, MBA-HM, BSN, RN,
Fresenius Home
Therapies Program Manager,
Fresenius Kidney Care

Donna Ferguson, RN, BSN
RN Charge
Nurse II,
Fresenius Kidney Care
This is In Person Session
The Mishawaka Indiana Home Therapy Team has operated on the premise that everyone deserves to attain their highest level of health and quality of life with improved dialysis treatment options. The Team aimed to cultivate a culture change and develop an effective strategy for delivering excellent kidney patient care.
A foundational component of the team’s strategy is based on Jean Watson’s Theory of Human Caring. In tandem with Watson's theory, the team integrated Lean Six Sigma principles into the framework.
This innovative process began in 2022 and incorporated elements into the new model, including group training, transforming traditional nursing roles, instilling an “owner versus renter” mentality, process improvement, and patient satisfaction through relationship-building practices. This foundation was designed to enhance the ability to deliver higher levels of care that improve the quality of life for every patient, every day.
During the group training implementation, clinical staff witnessed an exceptional phenomenon. Peer-to-peer relationships blossomed, spirits lifted, and the atmosphere in the room became magical. Patients were learning from each other and forming friendships that transcended the one-on-one training. Patients and caregivers began encouraging one another and forming their own support networks. The clinic’s dynamic was transformed because of it. Within the first 10 months, the number of trained patients surpassed the clinic's entire patient population from the previous year. This model of care is transformative and can lead to meaningful human connections that enhance the quality of care and improve a patient’s quality of life.
 April 8, 2024 14:00
April 8, 2024 14:00Using Community Health Assessments and Leveraging Community Resources to Improve Health Equity and Reduce Health Care Disparities

Linda Griskell, MHA (Moderator)
PATH Task Order
Director,
Comagine Health

Tasha Peltier, MPH, CPH
PATH
Quality Improvement
Advisor and Community Engagement Advocate,
Quality Health Associates of
North Dakota

Carrie Howard, MA, CPHQ, CPPS
PATH Quality
Improvement Advisor,
Stratis Health
Julia Drishinski, BSN, RN, CPHQ
PATH Quality
Improvement Advisor,
Mountain Pacific
This is In Person Session
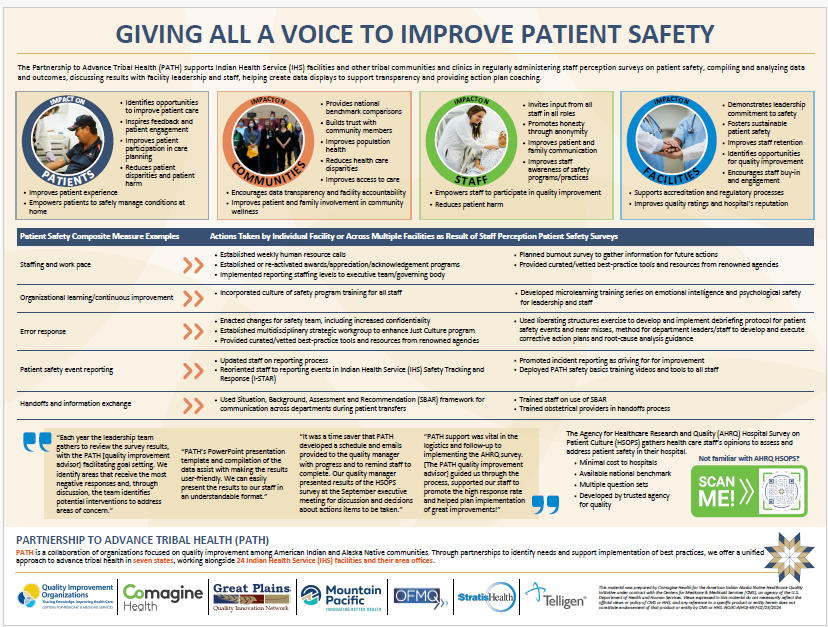
Four presenters, each a Partnership to Advance Tribal Health (PATH) team member
supporting a different
Indian Health Service (IHS) facility, will share their process, methods and goals for
supporting a
community in building a Community Health Assessments (CHA). Each presenter played a
different role in
the CHA process, illustrating how this work should be guided by each specific community
or group and how
trust, flexibility and responsiveness are keys to success in any initiative. Presenters
will share their
experiences, tools used, recommendations, challenges and successes for collaborating
with a tribal
community in building a CHA.
 April 8, 2024 14:00
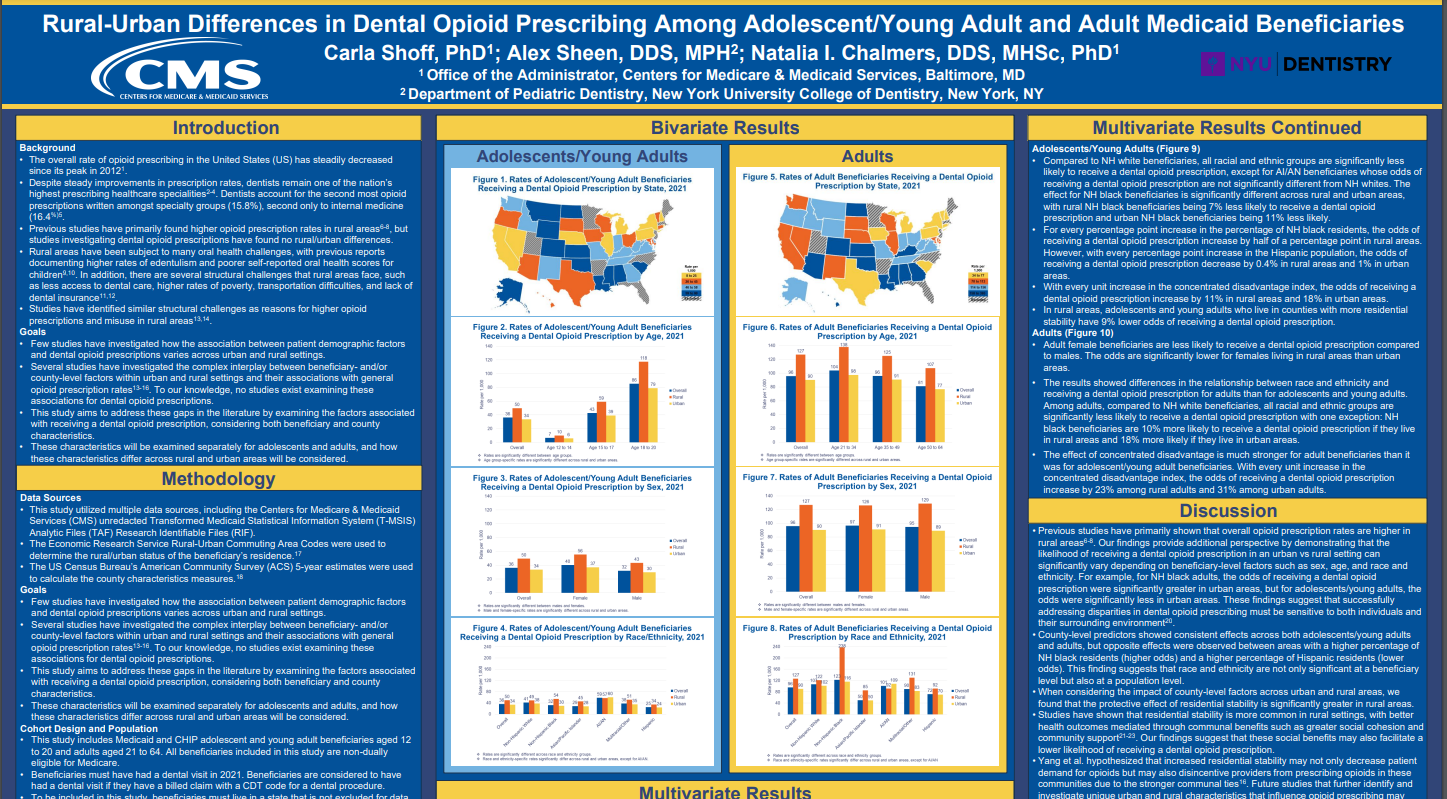
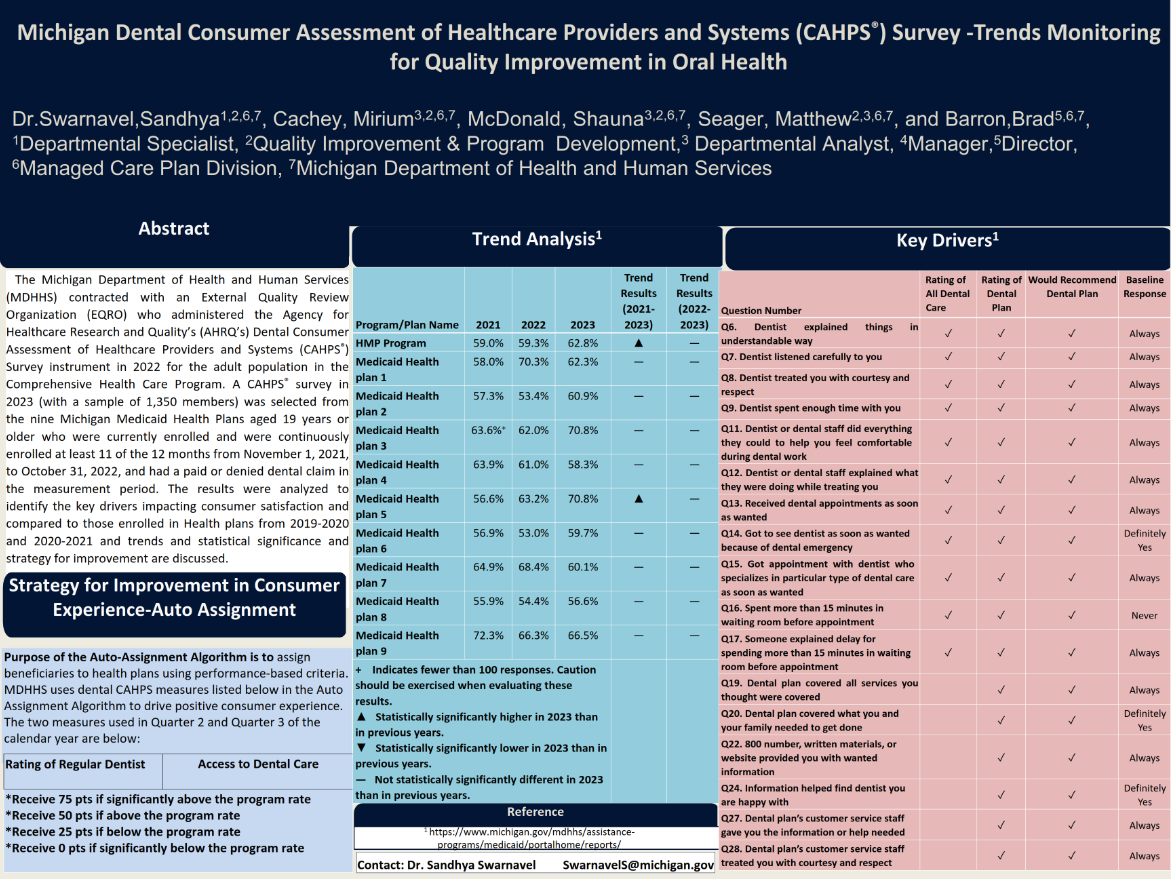
April 8, 2024 14:00Oral Health Quality Improvement in Medicaid and CHIP

Margo Rosenbach, PhD
Vice
President and Director of
Health Program Improvement,
Mathematica

Andrew Snyder, MPA, (Moderator)
Senior Policy
Advisor,
Center for Medicaid and CHIP Services,
Centers for Medicare
& Medicaid
Services
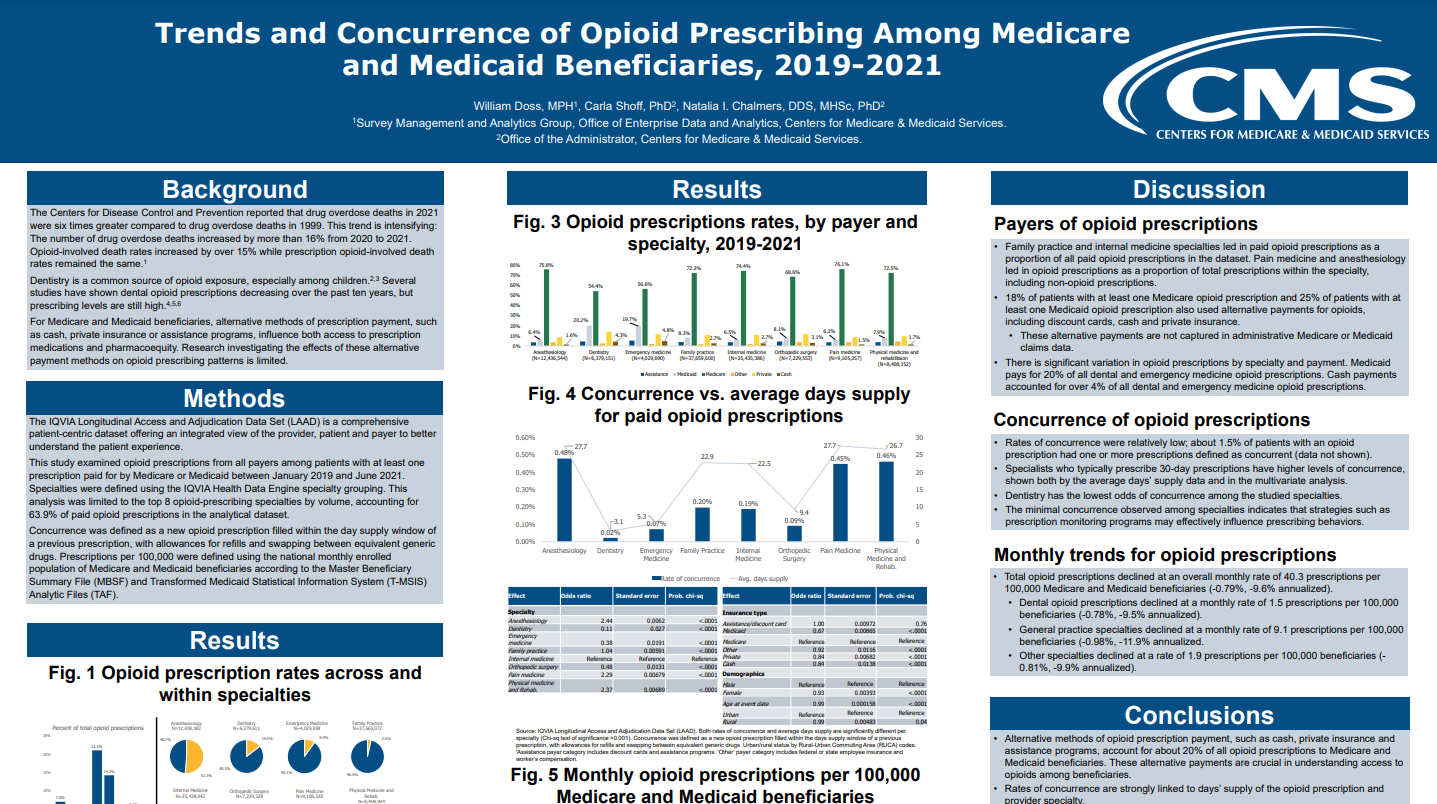
Natalia Chalmers, DDS, MHSc, PhD
Chief Dental
Officer,
Office of the Administrator,
Centers for Medicare &
Medicaid Services
This is In Person Session
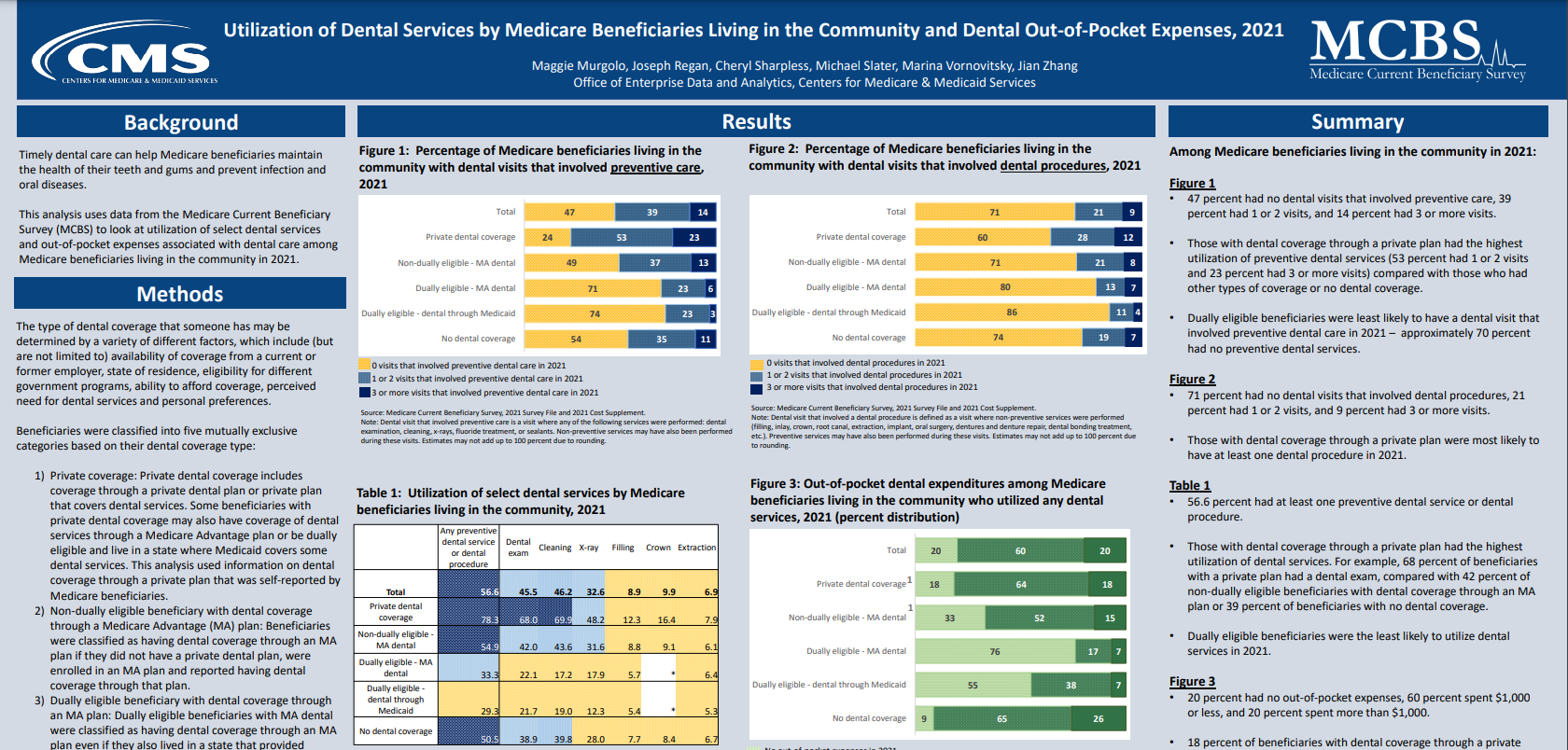
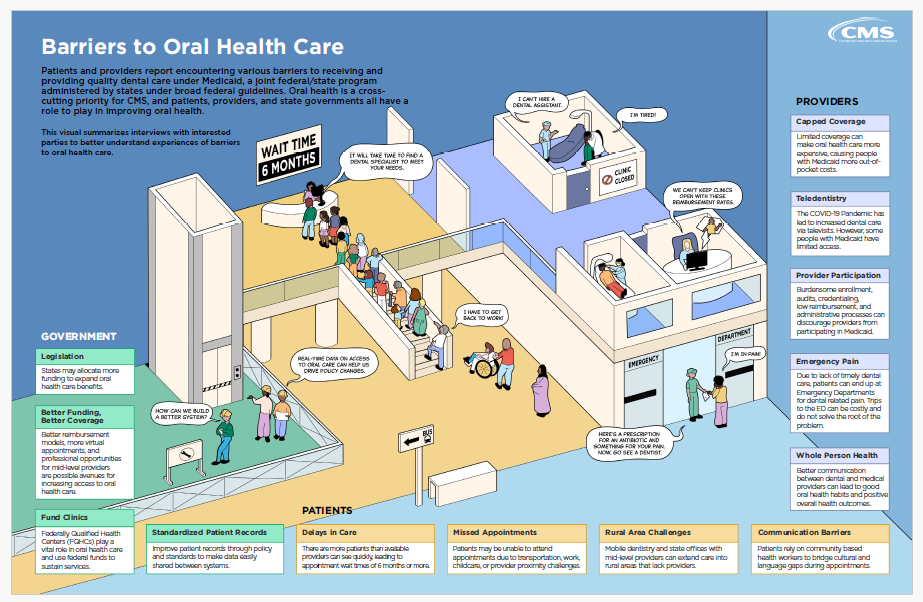
Over the past two years, CMS has made significant strides in advancing oral health across all our programs. From 2020-2023, a CMS learning collaborative focused on advancing oral health prevention in primary care. Topically applied fluoride varnish effectively prevents dental caries in children and adolescents. Because young children under 5 are more likely to see a primary care provider (PCP) than a dental provider, PCPs are uniquely positioned to support oral health prevention by offering fluoride varnish as part of primary care visits and connecting beneficiaries to dental care. The session will open with an overview of the technical assistance CMS provides state Medicaid and CHIP agencies and their quality Improvement (QI) partners to advance oral health prevention in primary care for Medicaid and CHIP beneficiaries, featuring several state QI projects from the affinity group, highlighting their strategies, partnerships, and lessons learned.
In 2022, CMS conducted its first-ever oral-focused human-centered design research in four states, interviewing nearly 100 people (i.e., beneficiaries, providers, advocates, state administrators, etc.) to understand barriers to oral health care access for the Medicaid and dually eligible population to inform policy change. In this session, The CMS Chief Dental Officer, Dr. Chalmers, will present the findings from that engagement.
CMS also convened a Workgroup to gather stakeholder feedback from experts in the field to plan strategic priorities for the next phase of our Medicaid and CHIP Oral Health Initiative. The focus is to assess gaps related to oral health and access to care for Medicaid and CHIP beneficiaries and recommend strategic priorities for the next five years. The session will conclude the workgroup process and overview of the final report and recommendations.
 April 8, 2024 14:00
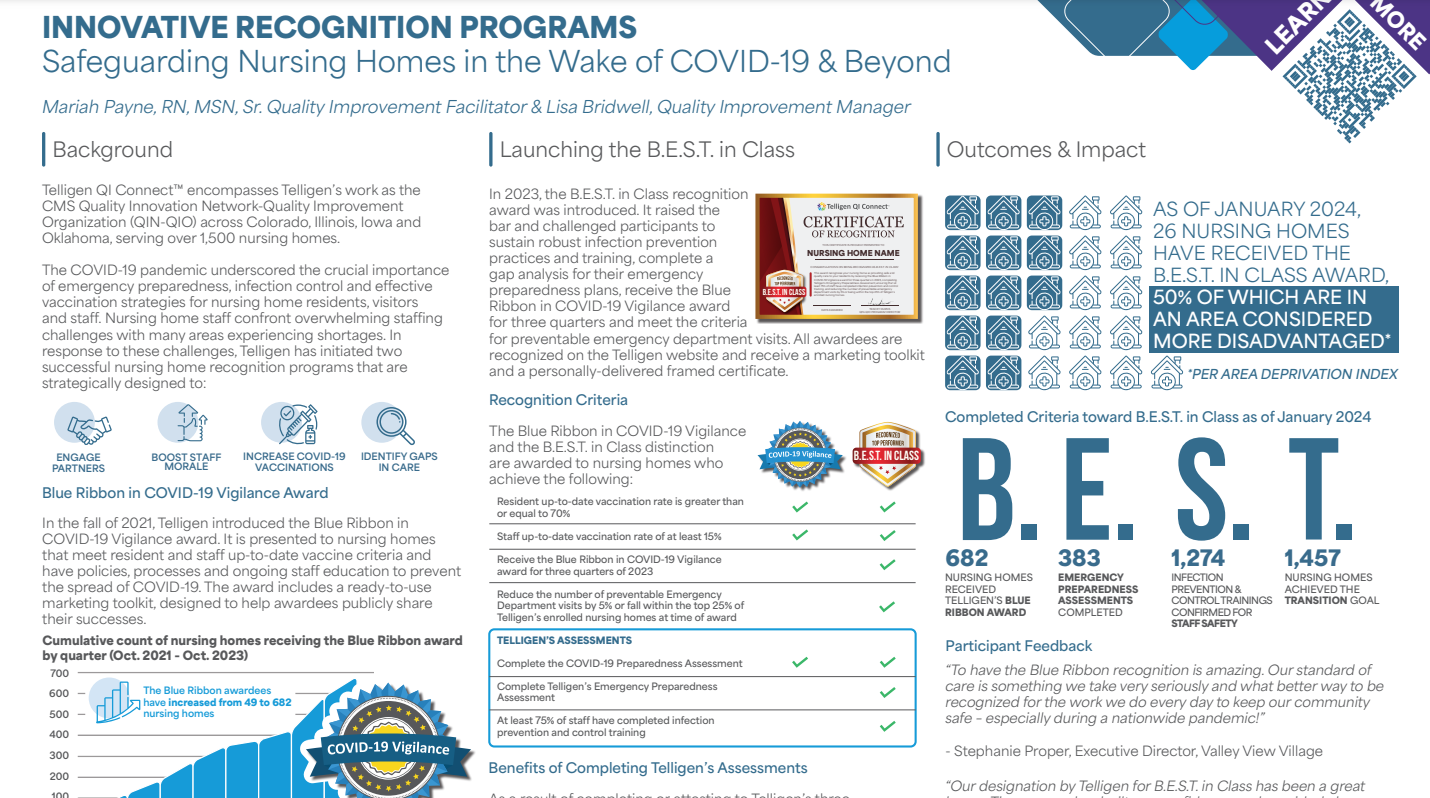
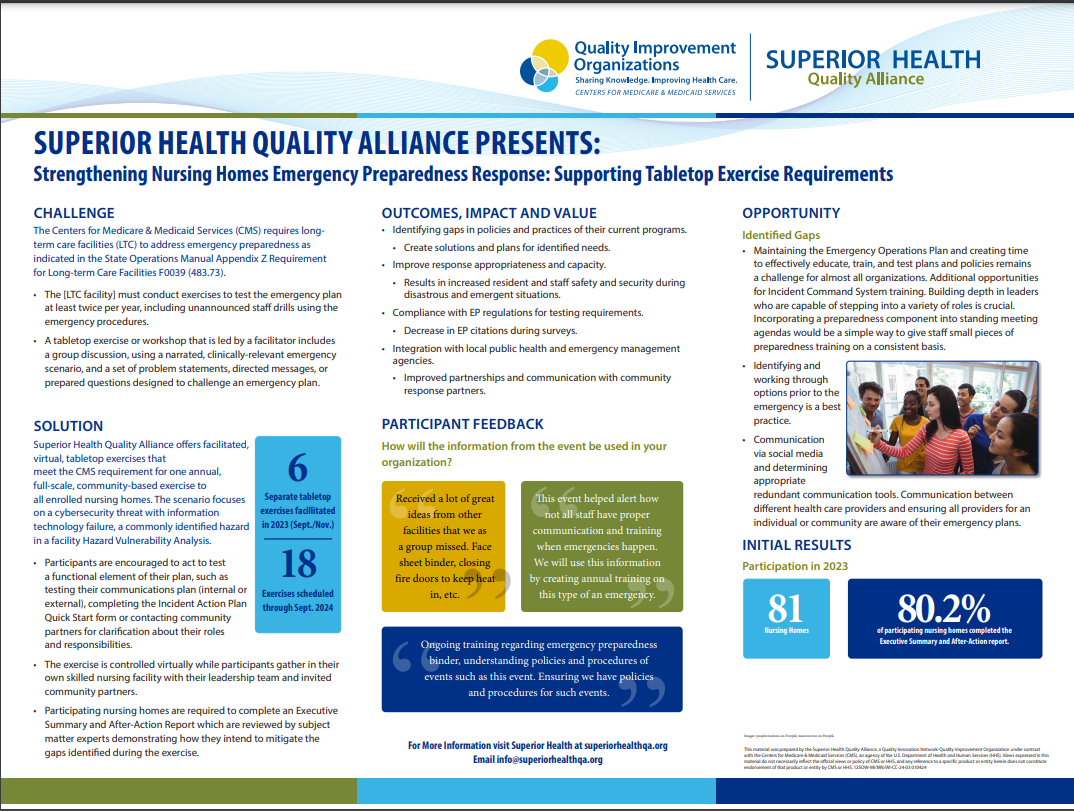
April 8, 2024 14:00Strengthening Nursing Home Emergency Preparedness: Insights from Telligen’s Online Assessment Tool and Collaborative Strategies for Resilience

Rejie Abraham, (Moderator)
Centers for Medicare
& Medicaid Services,
DCPH

Brian Feist, BSN, RN
Senior
Quality Improvement
Facilitator,
Subject Matter Expert for Emergency Preparedness,
Telligen
This is In Person Session
Emergency preparedness planning in nursing homes is crucial for safeguarding vulnerable populations, especially amid the challenges resulting from the pandemic. Staffing shortages limit the ability to focus on preparedness, with 77 percent of nursing homes facing challenges preparing for public health emergencies and natural disasters, according to a recent OIG report. To address this, Telligen developed an online assessment tool aligned with federal regulations and co-designed with nursing home partners to assist nursing homes in creating comprehensive emergency plans. This tool evaluates existing plans, procedures, and resources, focusing on evacuation plans, staff training, and essential resource availability and provides a comprehensive gap analysis for users to target their improvement efforts. Coordination with local emergency services for effective crisis collaboration is emphasized.
Upon completion, Telligen helps nursing homes identify and rectify gaps in their plans, enhancing their responsiveness to various emergencies. This session will highlight lessons learned from 368 completed assessments across a four-state region, showcase Telligen's collaboration with nursing home corporations to enhance testing, training plans, and system-level awareness for improvement, and offer best practices to foster a culture of readiness and resilience, ultimately ensuring the health and safety of residents and staff during crises.
 April 8, 2024 14:00
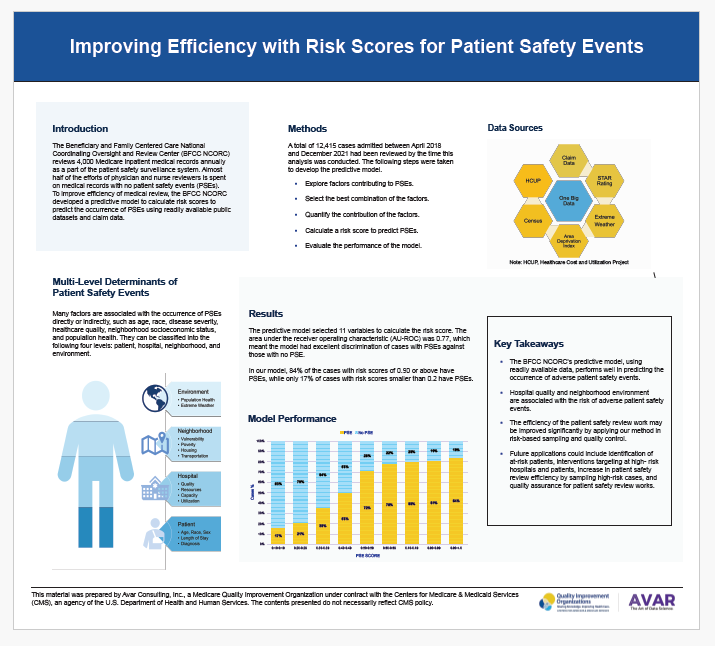
April 8, 2024 14:00The True Cost of Patient Safety Events and Pursuing the Goal of Zero Harm
Li Chen, Ph.D
Health Research
Lead,
Avar
Consulting

Wendy Gary, MHA, (Moderator)
Chief Operating
Officer,
Avar Consulting;
Executive Director,
BFCC-QIO;
Project Director,
BFCC
NCORC

Jacklyn Vollmer, MPH
Quality
Improvement and
Operations Support Specialist,
Avar Consulting
This is In Person Session
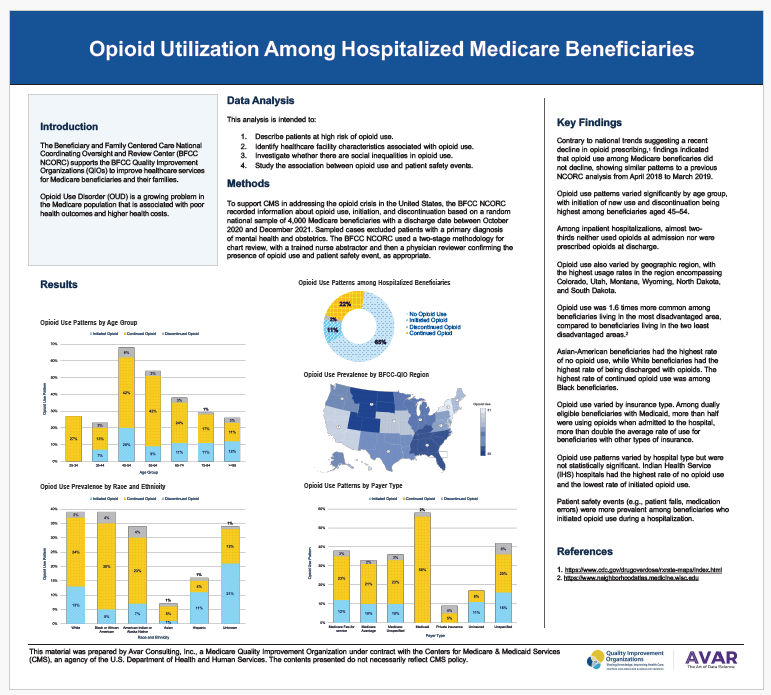
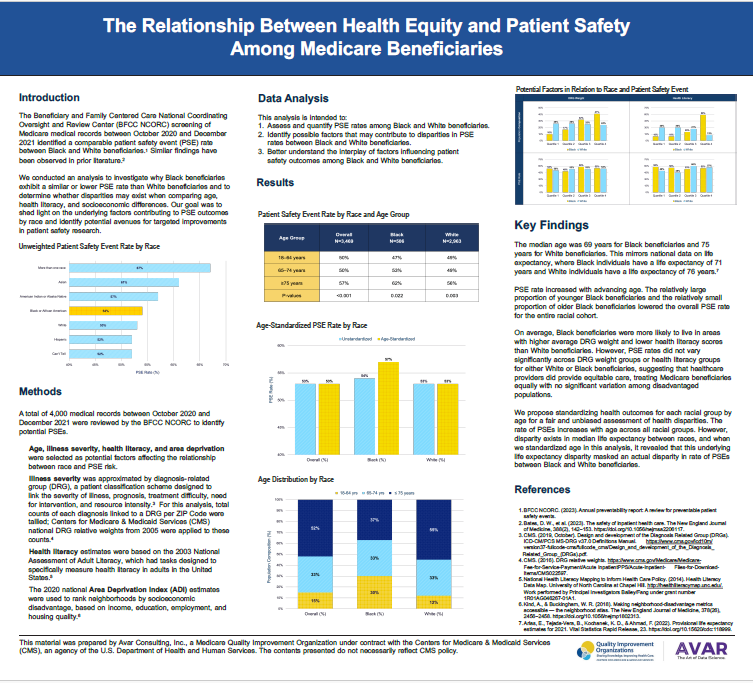
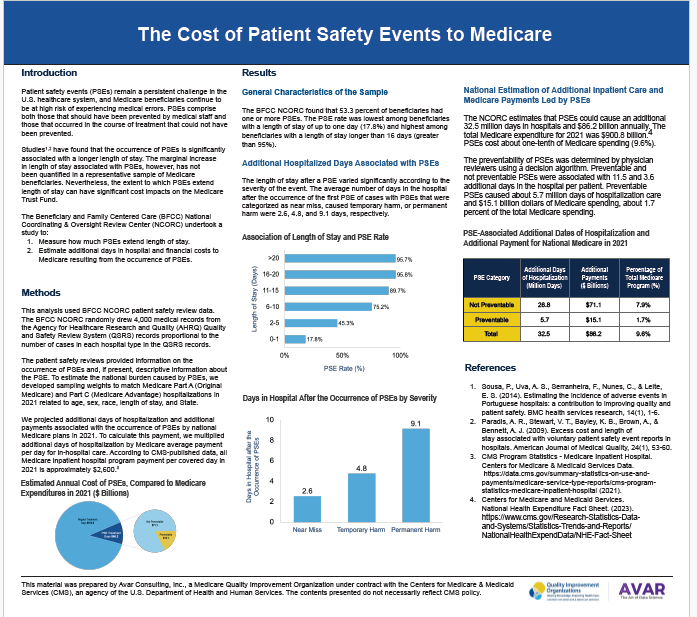
Patient safety events (PSEs) remain a persistent challenge in our healthcare system, and the Centers for Medicare & Medicaid Services (CMS) has adopted the goal of Zero Preventable Harm as part of its National Quality Strategy (NQS). This presentation will (1) discuss the prevalence of PSEs among Medicare beneficiaries, (2) analyze associated additional inpatient care and financial costs, and (3) provide insight to support CMS’ aim to promote the safest possible care for all. The Beneficiary and Family Centered Care National Coordinating Oversight and Review Center (BFCC NCORC) screens 4,000 Medicare medical records annually for PSEs, leading to follow-up actions by the BFCC-Quality Improvement Organizations (QIOs). NCORC analyzed additional days of hospitalization and payment associated with PSEs projected on a national level, by sample weighting, representing beneficiaries based on 4,000 Medicare discharges between October 2020 and December 2021. Over 5,000 PSEs were identified, and half of beneficiaries experienced at least one, with 6% being deemed preventable. PSEs were associated with nearly four additional days of inpatient care on average, totaling 32.5 million additional days nationally. This equates to $86 billion per year, or about one-tenth of all Medicare spending. Preventable PSEs cause about 5.7 million additional days of care, and over $15 billion in spending. Patient safety is the cornerstone of high-quality healthcare, yet PSEs happened in more than half of Medicare beneficiary hospitalizations, accounting for nearly 10% of all Medicare spending. These findings reinforce the urgent need for CMS’ quality agenda, and the goal of achieving zero preventable harm.
 April 8, 2024 14:00
April 8, 2024 14:00Introduction to Merit-based Incentive Payment System (MIPS) Cost Performance Measures

Allie Newsom, MPH
Senior Policy
Lead,
Acumen,
LLC

Christopher Reinartz, (Moderator)
Division
Director,
Information Systems Group,
Center for Clinical Standards
and Quality,
Centers for Medicare & Medicaid Services

Donta Henson, MS
Center for
Clinical Standards and
Quality,
Centers for Medicare & Medicaid Services

Shirley Fung, MPH, MSMR,
MIPS
Scoring, Data &
Analytics, and Operations Lead,
Center for Clinical Standards and
Quality,
Centers for
Medicare & Medicaid Services

Steven Szeliga, MS,
QPP Chief
Product Owner,
ICF International, Inc.
This session provides an overview of the Merit-based Incentive Payment System (MIPS) cost measure development process, measure methodologies (construction and attribution), cost measure scoring, and feedback reporting.
Cost measures are used to assess the overall cost related to providing and receiving medical care. Costs can include the direct costs of treatment, the total costs borne by a patient across all providers, follow-up care, outcomes after treatment, or some mixture of these. Cost measures are developed and maintained in iterative processes involving in-depth input from content experts and the public, such as Technical Expert Panels, Clinical Expert Workgroups, and persons and families with lived experience related to the cost measures. CMS uses Medicare administrative claims data to calculate cost measure performance, which means clinicians don’t have to submit any data for this performance category. MIPS eligible clinicians and groups who get scored on any of the cost measures will receive category and measure-level scoring information in their MIPS Performance Feedback Patient-Level Data Reports.
CMS will review an example of how a measure is developed, constructed, and scored. This will include defining an episode, identifying a clinician-patient relationship, determining the period of care, assigning costs of clinically related services, accounting for patient heterogeneity, calculating measure scores, and providing pertinent claims level feedback.
The session will provide insight on the methodologies CMS employs for developing and scoring cost measures, and how CMS is striving to improve the cost measures resources and data available to clinicians.
 April 8, 2024 14:00
April 8, 2024 14:00Who Seeks Medicare Support and Advocacy Services and How Can We Address Barriers and Reduce Disparities?

Scott Fortin, MBA
Sr. Director
Communications and
Outreach,
Kepro

Carmen Villegas, RN, BSN, BCPA
Immediate Advocacy
Manager,
Livanta

Stephanie Fry, BA, CPXP
Associate Vice
President,
Westat
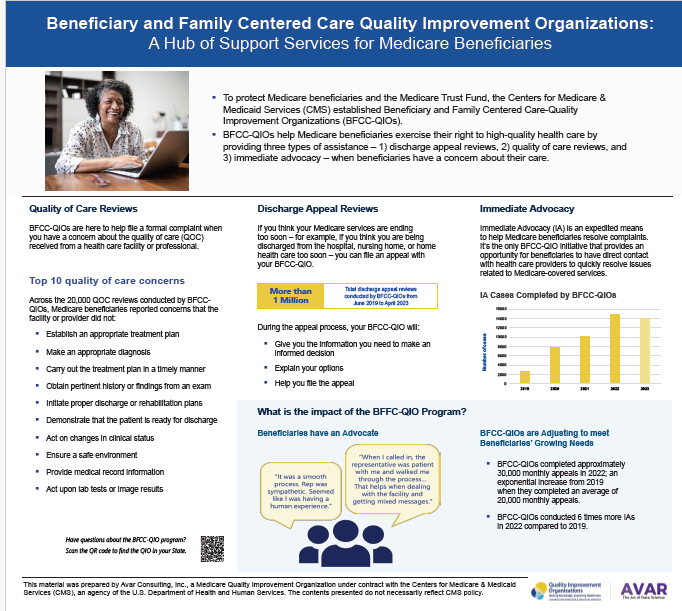
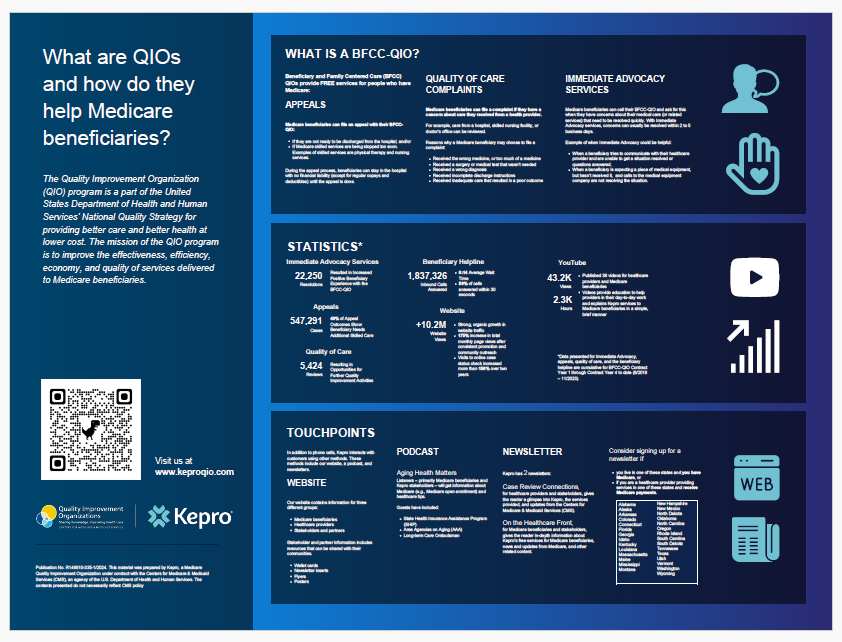
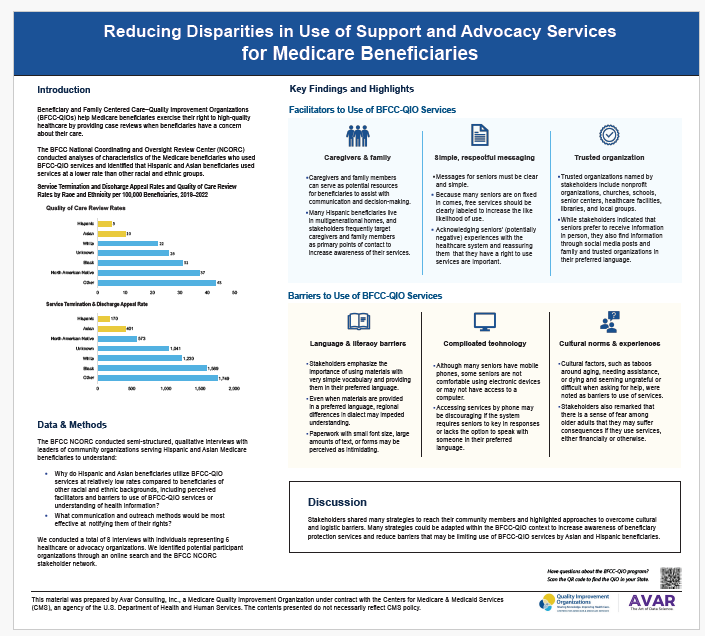
In response to the President’s executive order to advance racial equity and support for underserved communities, the Department of Health and Human Services (HHS) established an equity action plan. In alignment with this plan, Beneficiary and Family-Centered Care Quality Improvement Organizations (BFCC-QIOs) are working to identify and address barriers to equitable access and utilization of beneficiary protection, support, and advocacy services.
BFCC-QIOs offer case review services for beneficiaries who think they may be entitled to additional Medicare-covered services, or who think the quality of care they received does not meet clinical standards. Using BFCC-QIO program data, we assessed the degree to which case review services are being utilized by beneficiaries of different races and ethnicities.
Disparities in case review utilization are evident among Hispanic and Asian beneficiaries and these disparities may further contribute to existing health outcome inequalities. The concern is that these beneficiaries are still experiencing premature healthcare service termination or other quality of care issues such as gaps between government and other health providers, but are not exercising their right to review and possibly resolve these issues through BFCC-QIO program services.
BFCC-QIOs are carefully analyzing the approach and implementation strategies for their work. Seeking input from experts, stakeholders and Medicare beneficiaries, BFCC-QIOs are identifying strategies to improve access and awareness and reduce disparities in use of BFCC-QIO case review services that may contribute to poor health outcomes.
 April 8, 2024 14:00
April 8, 2024 14:00The 2024 National Impact Assessment Report – Collecting and Using Quality Data Across 26 CMS Programs

Robert Ziemba, PhD
Statistician,
HSAG

Kyle Campbell, PharmD
Project
Director,
HSAG

Kendra Hanley, MS, BA
Impact
Assessment Team
Lead,
HSAG
The 2024 National Impact Assessment aggregates retrospective data from 26 CMS quality and value-based incentive programs to characterize quality and efficiency impacts associated with the use of measures. The session will focus on summarizing key findings from these comprehensive analyses that provide important insights regarding effects of the COVID-19 pandemic during the period of analysis. We will describe national measure performance trend data pre-COVID-19 (2016–2019) compared with results in the initial years of the COVID-19 public health emergency (PHE)— 2020 and 2021— and describe patient impact and costs avoided when performance for select measures improved. Data also will be presented on how the CMS measure portfolio is evolving to reduce measurement burden and address CMS quality priorities. Lessons learned from the COVID-19 PHE and proposed actions to improve the resilience of quality measurement and the health care system will be discussed. Finally, underscoring equity as a primary objective of the CMS National Quality Strategy, the session will explore patterns of disparities in quality measure scores and offer insight into underlying drivers of disparities identified through focus groups in underserved communities.
 April 8, 2024 14:00
April 8, 2024 14:00Million Hearts 2027: Aiming for Impact with a Focus on Health Equity

Haley Stolp
Policy and
Partnership Strategist,
Centers for Disease Control Disease Control and Prevention
Laurence Sperling, MD, FACC, FAHA, FACP, FASPC
Executive Director,
Million Hearts Initiative,
Centers for Disease
Control and
Prevention

Taylor Streeter, MPH
Health
Scientist,
ASRT,
Inc.
Million Hearts® prioritized strategies for building healthy communities and optimizing
care through a
committed focus on specific populations experiencing inequities. This session describes
how Million
Hearts 2027 is addressing health equity with a review of communication assets and
opportunities for
engagement, an exploration of health equity-related issues for widespread use of
self-measured blood
pressure monitoring and cardiac rehabilitation, and an overview of new and future
opportunities to
reduce cardiovascular maternal health disparities.
 April 8, 2024 15:00
April 8, 2024 15:00Behavioral Health Integration: Innovation and Advancement in Primary Care

Elisabeth Kato, MD, MRP
Medical
Officer,
Agency for Healthcare Research and Quality

Shari Ling, MD (Moderator)
Deputy CMS Chief
Medical Officer,
Centers for Medicare & Medicaid Services

Michael Wittie
Public Health
Analyst,
Office of
Policy,
Office of the National Coordinator for Health Information
Technology

Rebecca VanAmburg
Social Science
Research
Analyst,
Center for Medicare and Medicaid Innovation,
Centers For
Medicare & Medicaid
Services

Karran Phillips, MD, MSc
Deputy
Director,
Center for Substance Abuse Treatment,
SAMSHA
This session will bring together experts in the field of Behavioral and Physical Health Integration from CMS’s Center for Medicare & Medicaid Innovation (CMMI), the Agency for Healthcare Research and Quality (AHRQ), and the Office of the National Coordinator for Health Information Technology (ONC) to discuss innovations and lessons learned. The speakers will share what they are doing in their specific areas and engage in discussion around 5 key elements of integration: 1) team based care, 2) workforce training, education and culture, 3) community and individual needs, 4) payment and 5) infrastructure, IT and data sharing.
Click Here to View Presentation
 April 8, 2024 15:00
April 8, 2024 15:00What Matters Most! A Patient Led Approach to Identifying and Prioritizing Patient Reported Measures of Safety, Diagnosis and Bias

Suz Schrandt, JD
Founder,
CEO
and Chief Patient
Advocate,
ExPPect

Martin Hatlie, JD
Founding
Member,
Patients
for Patient Safety US
This is In Person Session
This session will inform and engage participants in the development of Project PIVOT (Patients Involved in developing Outcomes Together), a patient-driven research initiative to identify and prioritize Patient Reported Experiences (PREs) and Patient-Reported Outcomes (PROs) that matter most to them on the issues of patient safety, diagnosis safety and health equity.
Purpose: There is heightened national awareness, including at the White House, across CMS and other DHHS agencies, and among researchers about improving patient experiences and outcomes by addressing embedded patient safety, diagnostic and health equity challenges. In the past, improvement work has incorporated traditional tools such as clinical outcome measures and satisfaction scores. There has been limited incorporation of PREs and PROs prioritized by patient/consumer community. Project PIVOT will provide an opportunity for a range of diverse patients/families, and communities, especially those who experience marginalization, to come together with measure development experts to identify and prioritize PREs and PROs that matter most to them.
Evaluation: The ultimate goal of Project PIVOT is to identify existing validated patient reported measures of patient safety and discrimination/bias and facilitate the creation of new validated measures where none exist to ensure more meaningful measurement and future research.
Outcomes:
- Patient-identified and prioritized, existing, validated PREs and PROs
- Patient-identified and prioritized PREs and PROs for which no validated measures exist
- PREs and PROs that address specific challenges faced by minorities, persons with disabilities or chronic conditions, persons at risk for disparate maternal/child health outcomes, and other communities at heightened risk for disparate outcomes.
 April 8, 2024 15:00
April 8, 2024 15:00Improving Healthcare Quality: Back to the Basics

Anita Monteiro
Director, iQuality
Improvement &
Innovation Group
Centers for Medicare & Medicaid Services

Joshua Cartwright, DHA, MHL, CPHQ, FACHDM
Associate Principal – HRC
Chartis

David Wright, MPA
Director,
Quality Safety
& Oversight Group,
Centers for Medicare & Medicaid
Services

Tom Evans, MD, FAAFP
President
& CEO,
Iowa
Healthcare Collaborative
This is In Person Session
Recognizing the scope and complexity of health system challenges can be overwhelming. Committing to improving quality in healthcare can be exciting but daunting. What does a successful path forward look like? As the PHE taught us, it’s the basics: consistent processes, quality monitoring and most importantly, staff engagement, that are at the heart of routine or extraordinary medical responses. This session will discuss how to focus on the basic systems and foundation necessary to build any quality intervention, both organizationally and personally. This session is focused on the power of personal purpose in shaping the path forward, and our collective responsibility in making and sustaining improvements.
 April 8, 2024 16:00
April 8, 2024 16:00Medicaid and CHIP Innovations in Postpartum Care Equity

Kristen Zycherman, RN, BSN
Quality Improvement
Technical Director,
Division of Quality and Health Outcomes, Children and
Adult Health Program
Group,
Center for Medicaid & CHIP Services
Adi Hirshberg, MD
Director of
Obstetrical Services,
Clinical Associate Professor, Maternal Fetal Medicine,
Hospital of the
University of
Pennsylvania, Penn Medicine

Lindsay Standeven, MD
Assistant
Professor of
Psychiatry and Behavioral Sciences and Clinical Education Director,
The
Johns Hopkins
Reproductive Mental Health Center
This is In Person Session
This session will focus on the Equity in Postpartum Care Challenge prize competition, which rewards innovative strategies to improve postpartum care for Black or African American and American Indian or Alaska Native (AI/AN) beneficiaries enrolled in Medicaid or Children’s Health Insurance Program (CHIP). The competition emphasizes follow-up care form conditions associated with morbidity and mortality in the later postpartum period, including diabetes, postpartum depression and/or postpartum anxiety, hypertension, and substance use disorders (SUD). Two winners will speak about their winning projects and how they succeeded in scaling and spreading their ideas to improve equity in postpartum care.
 April 8, 2024 16:00
April 8, 2024 16:00Quality Oversight of Medicaid Home and Community-based Services (HCBS) Waivers

George Failla, Esq.
Director,
Medicaid &
CHIP Operations Group,
Division of Home and Community Based Services
Operations and
Oversight,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services

Susan Cummins
Technical
Director,
Medicaid
& CHIP Operations Group,
Division of Home and Community Based
Services Operations and
Oversight,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services
This is In Person Session
This session will provide information about the statutory and regulatory quality requirements associated with HCBS waiver programs. The session will outline the quality assurances states must provide, including obligations for quality monitoring and improvement. It will also provide details about the Center for Medicaid and CHIP Services quality oversight including health and welfare site visits in states.
 April 8, 2024 16:00
April 8, 2024 16:00Improving Care for People with Sickle Cell Disease:CMS & NIH/NHLBI Updates

Teanika Hoffman, MA
CHW,
Sickle Cell Coalition
of Maryland

Shondelle Wilson-Frederick, PhD, NHLBI
Chief
Engagement Officer,
National Heart, Lung and Blood Institute (NHLBI)
National Institutes
of Health (NIH)

Melissa Majerol
Cell and Gene
Therapy Access Model
Co-Lead,
Center for Medicare and Medicaid Innovation (CMMI)

Jessica Lee, MD, MSHP
Acting
Chief Medical
Director,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services
This is In Person Session
This session will focus on efforts from CMS and NIH/NHLBI to improve access, quality, and the experience of health care for individuals with Sickle Cell Disease (SCD). In 2023, CMS released a new CMS Action Plan for SCD. The Action Plan is based on listening sessions and lessons from the field as CMS is continuously gathering information on what barriers exist for individuals and providers. CMS will highlight some activities in the SCD Action Plan that address the challenges specific to CMS programs which are designed to improve health outcomes and reduce health disparities for individuals with SCD. In addition, this session will address current NIH/NHLBI efforts that are underway to advance our research and knowledge of SCD to help improve the lives of those living with this disease. Lastly, you will hear from a representative from the Maryland Sickle Cell Disease Association and her experience with SCD.
 April 8, 2024 16:00
April 8, 2024 16:00Considerations for Developing New Measures in CMMI Models Highlighting Integrated Care for Kids and Emergency Triage

Alexis Lilly, MBA
Deputy
Director,
Center for
Medicare and Medicaid Innovation (CMMI),
Centers for Medicare &
Medicaid Services

Chadwick Morgan, MPH
Integrated
Care for Kids
Center for Medicare and Medicaid Innovation (CMMI)
Centers for
Medicare & Medicaid
Services

Emily Creveling, MSW
Integrated
Care for Kids Model
Co-Lead,
Center for Medicare and Medicaid Innovation (CMMI),
Centers
for Medicare &
Medicaid Services

Jacob Quinton, MD, MPH
Medical
Officer,
Center
for Medicare and Medicaid Innovation (CMMI),
Centers for Medicare &
Medicaid
Services

Marvin Nichols, MHA
ET3 Model
Lead,
Center for
Medicare and Medicaid Innovation (CMMI),
Centers for Medicare &
Medicaid Services
This is In Person Session
As CMS seeks to align quality measures through the Universal Foundation, there remain important measurement gaps. The CMS Innovation Center strategically chooses to develop new measures when tied to the overarching goal of a model. We will describe the context, importance and development of new measures for Center for Medicare and Medicaid Innovation (CMMI) alternative payment models.
CMMI will discuss considerations for new measure development in newly announced CMMI models, as well as the approach and rationale for new measure development in current models. This session will also highlight novel measures under the Integrated Care for Kids (InCK) and Emergency Triage, Treat, and Transport (ET3) model and the Guiding an Improved Dementia Experience model to highlight this work:
InCK: There is evidence that interventions aimed at reducing rates of youth out of home placement (OOHP) have the potential to both improve children’s health outcomes and reduce their rates of avoidable health care utilization. This session will provide an overview of the novel OOHP measure developed for the InCK Model. This measure reports the rate of new OOHP episodes per 1,000 attributed beneficiaries in a set geographic area.
ET3: The ET3 Model tested an innovative new approach to paying for emergency ground ambulance services in Medicare. In order to better assess the efficacy of triage interventions, CMMI developed the Post-Triage Emergency Department (ED) Visit measure that assessed the rate at which patients return to the ED within three days of an intervention.
Participants will learn how the CMS Innovation Center evaluates opportunities to develop new quality measures and the details of recently developed measures.
 April 8, 2024 16:00
April 8, 2024 16:00Addressing Health-Related Social Needs of Patients with Kidney Disease

Sonya Streeter, MPP, MPH
Associate Vice
President,
Westat

Chiao Wen Lan, PhD, MPH, CPH
Social Scientist,
End Stage Renal Disease National Coordinating Center (ESRD NCC)
This is In Person Session
A critical part of advancing reform and addressing provider burden in the health care system is creating meaningful alignment among payers. Over the last year, both Center for Medicare and Medicaid Innovation (CMMI) and the Learning and Action Networks (LAN) have announced new models and initiatives meant to generate directional alignment that balances the need for multi-payer alignment goals with payer flexibility. This session describes how these efforts work together to generate this alignment at both the national and local levels.
Emphasizing both collaborative and individual efforts, CMMI and the LAN will highlight key initiatives and milestones generating meaningful multi-payer alignment across the healthcare market. In both instances, these efforts adopt the principles of directional alignment, where alignment does not require identical arrangements or programs, but looks to create collaboration and alignment around core areas, such as quality measurement, and create closer alignment over time.
Participants will learn how CMMI and the LAN are working together and with a wide range of partners to advance alignment in key areas of delivery system reform.
 April 8, 2024 16:00
April 8, 2024 16:00Case Studies to Reduce Hospital-Acquired Infections Through Group Peer-to-Peer and 1:1 Customized Technical Assistance

Donna Cohen, BSN, RN, CCM
Director Quality
Programs,
Alliant Health Solutions

Rose Langdon, BSN, MBA, CPHQ, FNAHQ
Lead
Educator,
TMF Health Quality Institute

Karen Holtz, MS, MT(ASCP), CPHQ
HQIC Education
Lead,
Alliant Health Solutions

Ann Werner, MSW, CPHQ
Director,
TMF Health
Quality Institute
In the aftermath of the COVID-19 pandemic, hospitals struggled with low performance in healthcare-associated infections (HAIs). Hospitals were overwhelmed and frustrated with their performance as a result of competing priorities due to COVID-19 and resultant staff turnover. Health care professionals, specifically infection preventionists (IPs) struggled during and after the pandemic.
In 2023, TMF launched a series of topic-specific affinity discussion groups to address lagging performance by its supported hospitals on specific patient safety measures. Each affinity group met monthly for three months and focused on one specific topic. We started with topics that hospitals struggled to improve, such as sepsis and pressure injuries. We provided short on-demand videos, tools and resources, and access to a subject matter expert for each group. The theme of Cultivate Your Patient Safety Environment was used across all affinity group topics.
The Alliant Hospital Quality Improvement Contractor (HQIC) applied a peer-to-peer strategy through hospital networking and one-on-one customized calls to reduce HAIs as well as improve reporting of National Healthcare Safety Network (NHSN) data. As a result of a networking call, one hospital was able to learn from a high performing hospital to significantly decrease pressure injuries. An Infection Preventionist and subject matter expert worked one-on-one with hospitals that had newly hired IPs or staff new to the role. Together, they identified gaps and implemented interventions that led to change and improvement in HAIs. Coaching packages which included best-practice interventions and links to relevant resources and professional websites were shared with hospitals. The data were monitored over time until target goals were achieved.
 April 8, 2024 16:00
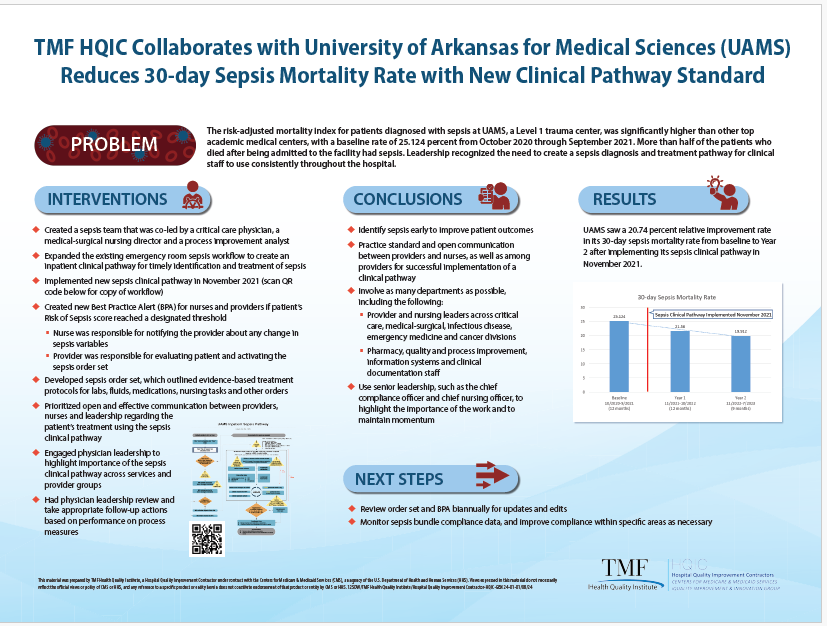
April 8, 2024 16:00Building the Foundation of a Strong Hospital Sepsis Program to Optimize Patient Care and Improve Outcomes

Virginia Brooks (Moderator) MHA, CPHQ, FACHE
Vice
President,
Health Quality Innovators

Rebecca Boll, MSPH, CPHQ
Senior
Director,
IPRO

Charisse Coulombe, MS, MBA, CPHQ, CPPS
Director,
Hospital Quality Initiatives,
Iowa
Healthcare Collaborative
(IHC)

Kendra Cooper, MSN-HCQ, RN, CPHQ
Consulting
Manager,
Health Quality Innovators

CarlaLisa Rovere-Kistner LCSW, CPHQ, CCM
Quality
Improvement Specialist,
IPRO
This is In Person Session
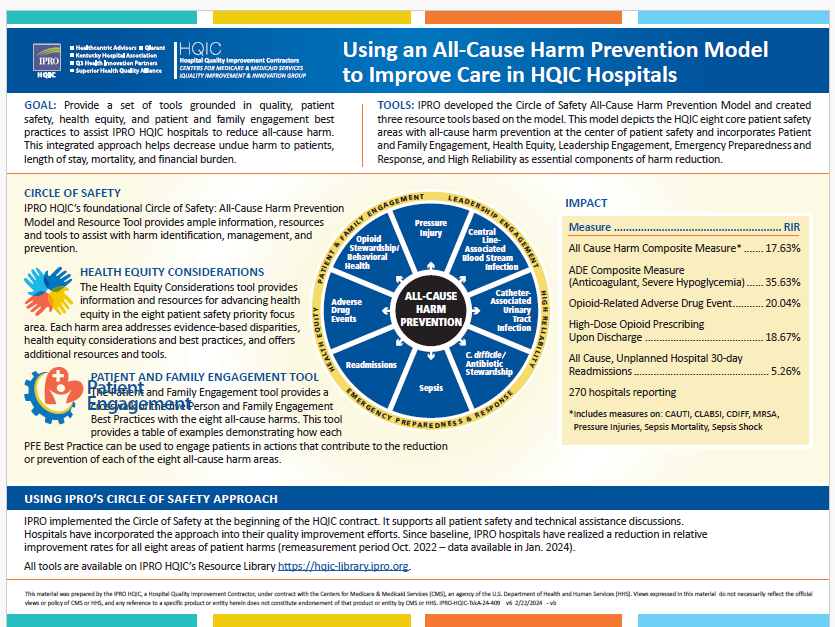
Hospital Quality Improvement Contractor (HQIC) use a variety of data sources to inform their ability to provide customized technical assistance. As early adopters and promoters of the Centers for Disease Control and Prevention (CDC) Hospital Sepsis Program Core Elements, Health Quality Innovators (HQI) leveraged this framework to identify hospital program needs and designed a flexible core of technical assistance to meet hospitals at various levels of sepsis program implementation. Health Quality Innovators (HQI) analyzed the NHSN 2022 Patient Safety Component—Annual Hospital Survey, specifically responses under the Sepsis Management and Practices section. Questions in the annual survey are closely tied to the CDC’s Hospital Sepsis Program Core Elements, however, Health Quality Innovators (HQI) was already using this framework with HQIC hospitals prior to the official launch of the program in August 2023. Health Quality Innovators (HQI) used the survey results to inform technical assistance planning and one-on-one coaching. IPRO also created a sepsis gap assessment to obtain an in-depth understanding of the hospitals’ needs. This gap assessment was then used to inform education needs and content for inclusion in a sepsis affinity group. In addition, IHC created and utilized low performer reports to identify the hospitals and specific components in the greatest need for technical assistance and sepsis education. All three Hospital Quality Improvement Contractors (HQICs) use Medicare FFS Administrative Claims data and site visits to measure improvement in sepsis mortality. Approximately 669 hospitals enrolled in either the Health Quality Innovators (HQI), IPRO or IHC, Hospital Quality Improvement Contractor provider engaged in a variety of interventions to reduce sepsis mortality over three years of the Hospital Quality Improvement Contractor project. These interventions included change pathways, affinity groups, action plans, office hours, educational events, podcasts, site visits and survivor stories. Several initiatives were expanded to include collaboration with additional Hospital Quality Improvement Contractors. During this session, we will highlight both Hospital Quality Improvement Contractor wide interventions as well as specific case studies describing specific systems, processes, and strategies that attributed to improvements in sepsis care and reduced mortality.
 April 8, 2024 16:00
April 8, 2024 16:00Demonstrating Attributable Impact in Quality Improvement Through Success Stories

McCall Glover, MPH
Data
Scientist,
Booz Allen
Hamilton
In May 2023, the Independent Evaluation Contractor (IEC) hosted a roundtable discussion with representatives from all 12 Quality Innovation Network – Quality Improvement Organizations (QIN-QIO) contractors; the discussion aimed to understand how contractors define, measure, and report attributable impact within individual healthcare environments. Findings from the 2023 closed-door session and subsequent follow-up data were analyzed. Insights pertaining to alignment of success definitions informed the development of CMS resources to support contractors’ use of success stories to support assessment of attributable impact.
The goal of this IEC presentation is to share progress toward adequately identifying and reporting success stories in quality improvement that suggest that provider impacts may be attributable to the contractors’ support.. The IEC will present analyses from QIN-QIO-furnished qualitative data related to identified cases of observed healthcare improvement collected during the NQIIC 12th SOW, November 2019 through November 2023. Findings include QIN-QIO feedback on challenges in capturing their own success and opportunities for improving the definition of success. The IEC will discuss lessons learned and next steps to help QIN-QIOs improve the process of identifying and communicating evidence of attributable impact.
 April 8, 2024 16:00
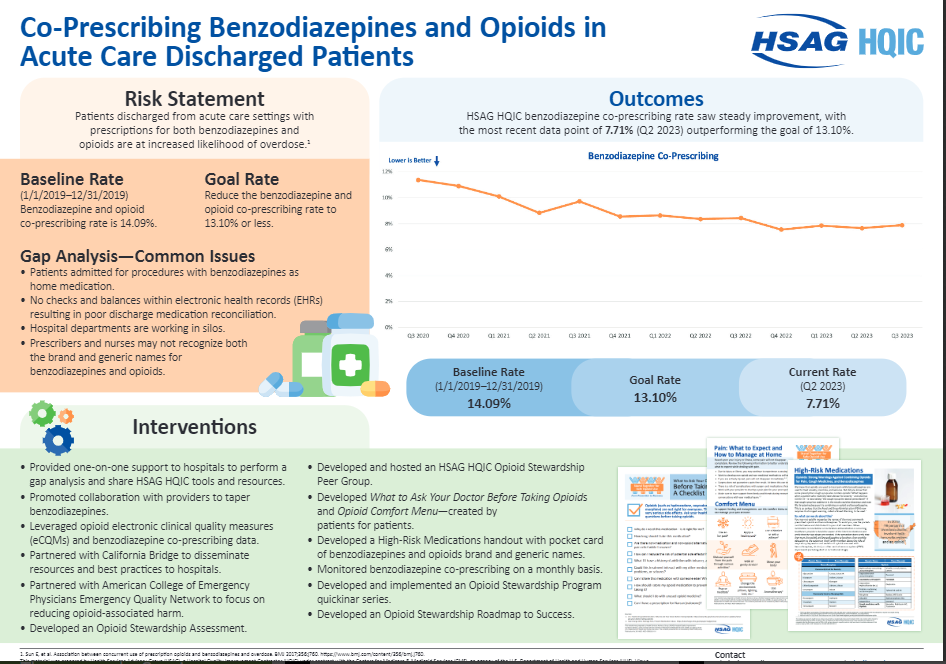
April 8, 2024 16:00Chronic Pain: Getting People the Care and Services they Need

Paige Mathew, PharmD, BCPS, BCGP
Pain Management
and Opioid Stewardship Clinical Pharmacy br/>Program Manager, Department
of Veterans
Affairs

Scott Lawrence, DC, CHCQM, FABQAURP
Senior
Advisor,
CMS Quality Improvement and Innovation Group

Tara McMullen, PhD, MPH
Associate
Director Opioid
Safety,
Veterans Health Administration
This is In Person Session
More than one fifth of American adults live with chronic pain, with about seven percent experiencing “high impact” pain. In US military veterans, chronic pain is even more common, with nine percent suffering from severe pain. Pain is a debilitating condition that negatively affects quality of life and work and is closely associated with depression, dementia, suicidality, and substance use. Pain also disproportionally impacts people who are racial and ethnic minorities, bisexual, divorced/separated, living with a disability, and have chronic conditions like arthritis and kidney disease. Nearly 80 percent of people with Medicare report chronic pain that interferes with function. Pain causes disability and social isolation, and is an ongoing burden for individuals, families, friends, caregivers, and health systems. Advancing pain care across all groups, ages, and settings is a public health imperative. Addressing pain effectively is one of the four goals of CMS’s Behavioral Health Strategy, prompting new monthly payment codes to help people with Medicare more easily access holistic care in an ongoing clinical relationship. The Department of Veterans Affairs (VA) has a long history of developing successful solutions for pain management. Its Stepped Care Model of Pain Management is one example and there is new work in pain measurement that offers potential to better tailor care. The person-centered and team-based approaches employed by the VA can serve as a model for other health systems seeking feasible, effective pain care that improves lives.
 April 8, 2024 16:00
April 8, 2024 16:00Quality Framework for a High Reliability Organization (HRO)

John Sellner, PharmD
Association Director of
Quality and Safety,
Minnesota Hospital

Roderick Baker
Associate Vice
President of
Development,
Winona Health
This is In Person Session
The road to becoming a High Reliability Organization (HRO) can be long and complex. The Minnesota Hospital Association (MHA) saw the desire from Minnesota hospitals and health systems to begin their HRO journeys and, using their unique process to tackle quality improvement, developed a strategic process for implementing and rolling out an HRO program. MHA created a road map for their members to use to successfully implement their own HRO program from getting started, all the way through advanced HRO implementation. MHA’s Director of Quality and Safety, John Sellner, PharmD, RPh, will present on MHA’s strategic process to tackling quality and the implementation and rollout of the High Reliability Road Map. Roderick Baker, Winona Health Minnesota will review Winona Health’s utilization of the Road Map in their HRO journey and provide recommendations to participants on how to utilize HRO resources to inform learnings and make improvements along the way.
 April 8, 2024 16:00
April 8, 2024 16:00Resilient and Ready Together: Applying a Community Informed, Geographic Lens to our Work

Kitichia Weeks, MA
Health
Insurance
Specialist/Account Manager,
Division of Health Plans Operations,
Centers for Medicare
& Medicaid Services
Thomas Bane, PhD, LMSW
Special
Assistant to the
Regional Administrator,
OPOLE,
Centers for Medicare & Medicaid
Services

Ashby Wolfe, MD, MPP, MPH
Regional Chief Medical
Officer,
Center for Clinical Standards and Quality,
Centers for
Medicare & Medicaid
Services

Susan Karol, MD
Chief Medical
Officer,
Division of Tribal Affairs,
Centers for Medicare & Medicaid
Services
This is In Person Session
This session will provide an overview of the CMS Framework for Advancing Health Care in Rural, Tribal, and Geographically Isolated Communities and how it supports CMS’s overall efforts to advance health equity, expand access to quality, affordable health coverage, and improve health outcomes for all Americans. The Framework’s six priorities were identified through lessons learned and feedback from those living and working in rural, Tribal, and geographically isolated communities. CMS’s approach to operationalizing this Framework over the next five years will be informed by ongoing public engagement, as appropriate, and CMS will continue to monitor trends in health and health care that uniquely impact rural, tribal, and geographically isolated areas.
 April 8, 2024 16:00
April 8, 2024 16:00Oral Health Quality Improvement in Medicaid and CHIP

Margo Rosenbach, PhD
Vice
President and Director
of Health Program Improvement,
Mathematica

Andrew Snyder, MPA, (Moderator)
Senior Policy
Advisor,
Center for Medicaid and CHIP Services,
Centers for Medicare
& Medicaid
Services
Over the past two years, CMS has made significant strides in advancing oral health across all our programs. From 2020-2023, a CMS learning collaborative focused on advancing oral health prevention in primary care. Topically applied fluoride varnish effectively prevents dental caries in children and adolescents. Because young children under 5 are more likely to see a primary care provider (PCP) than a dental provider, PCPs are uniquely positioned to support oral health prevention by offering fluoride varnish as part of primary care visits and connecting beneficiaries to dental care. The session will open with an overview of the technical assistance CMS provides state Medicaid and CHIP agencies and their quality Improvement (QI) partners to advance oral health prevention in primary care for Medicaid and CHIP beneficiaries, featuring several state QI projects from the affinity group, highlighting their strategies, partnerships, and lessons learned.
In 2022, CMS conducted its first-ever oral-focused human-centered design research in four states, interviewing nearly 100 people (i.e., beneficiaries, providers, advocates, state administrators, etc.) to understand barriers to oral health care access for the Medicaid and dually eligible population to inform policy change. In this session, The CMS Chief Dental Officer, Dr. Chalmers, will present the findings from that engagement.
CMS also convened a Workgroup to gather stakeholder feedback from experts in the field to plan strategic priorities for the next phase of our Medicaid and CHIP Oral Health Initiative. The focus is to assess gaps related to oral health and access to care for Medicaid and CHIP beneficiaries and recommend strategic priorities for the next five years. The session will conclude the workgroup process and overview of the final report and recommendations.
 April 8, 2024 16:00
April 8, 2024 16:00Bridging the Gaps in the Kidney Transplant Journey: Innovation Collaborations in CKD, Dialysis and Transplant

Victoria Cash MBA, BSN, RN, CPHQ
Executive
Director,
IPRO ESRD Network of the Ohio River Valley

Ivory Harding, MS
Director,
Quality and
Regulatory Affairs,
National Kidney Foundation

Matthew Cooper MD
Chief of
Transplantation,
Director of the Solid Organ Transplant Line and Professor of Surgery at the
Medical College of
Wisconsin,
Medical College of Wisconsin

Sherri Morgan-Johnson RN, BSN, MHSA, FAC-COR III
Nurse Consultant,
Centers for Medicare &
Medicaid Services

Sumeska Thavarajah, MD
Medical
Director,
Fresenius Kidney Care

Charles Rice, CPhT, MTM, BBM
ETCLC National
Faculty, Patient and Family Representative
During this patient-centered roundtable session, attendees will learn from kidney dialysis/transplant patients, the NKF, ESRD Networks, QIN-QIOs, TAQIL, and experts as they explore the complete kidney transplant journey.
From the five CKD stages to dialysis treatment options, and the transplant process, the expert panel will highlight gaps throughout the transplant care continuum and identify potential solutions, including strategies to reduce inequities experienced by underserved communities.
To address these identified gaps, speakers will review available partnership opportunities, new programs being tested in select communities, critical resources accessible to healthcare professionals, as well as the vital need to improve patient education that is culturally and linguistically appropriate throughout the kidney care system.
 April 8, 2024 16:00
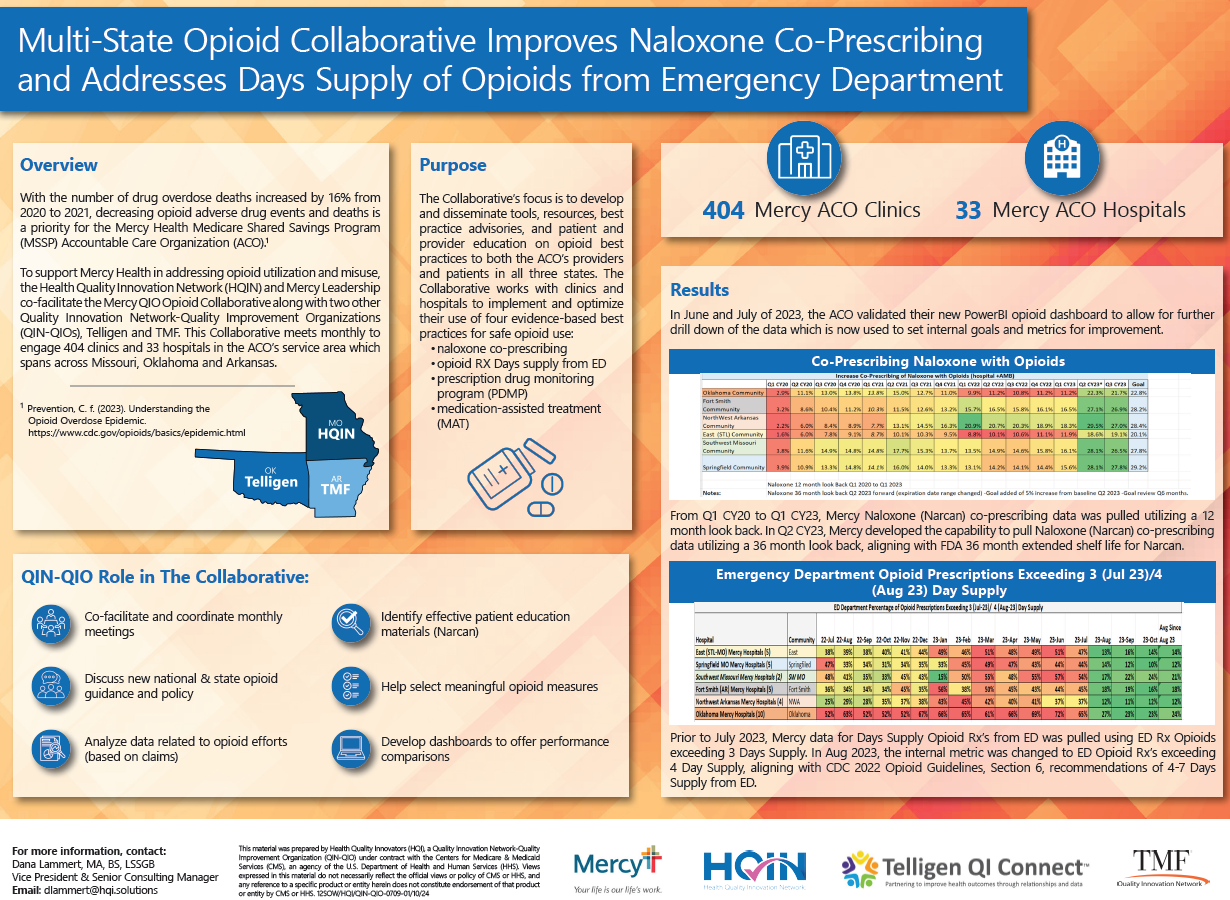
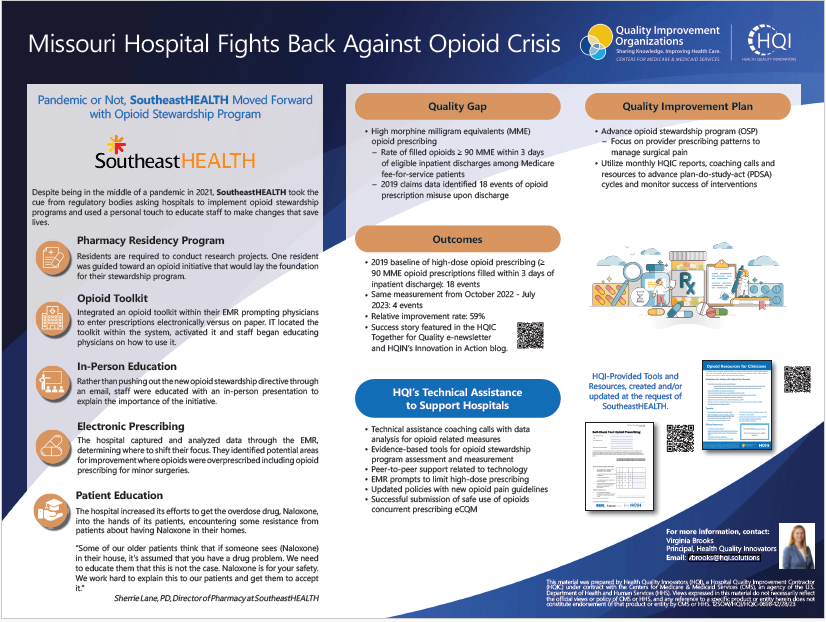
April 8, 2024 16:00HHS’ Call to Action on Opioid Use Disorder Treatment
This is In Person Session
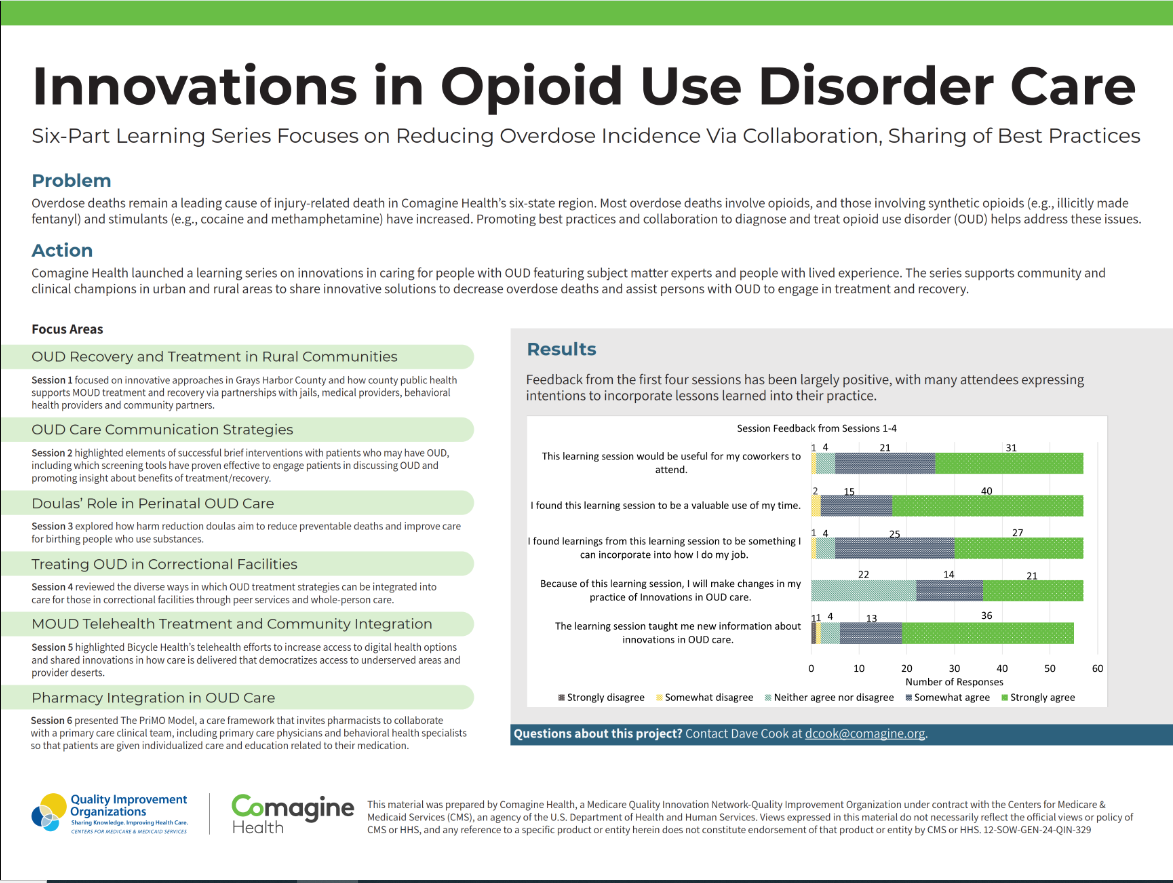
Drug overdose deaths in the United States, driven by illicit fentanyl and other opioids, remain at historically high levels – with more than 107,000 lives lost in the past year, and millions more struggle with opioid and other substance use disorders. The opioid crisis reaches every corner of our country, from alleyways to nursing homes, and requires an immediate call to action. Federal partners, local governments, healthcare institutions, and communities are working together to provide viable solutions to combating the opioid crisis.
There is a nationwide need for education on medications for opioid use disorder (MOUD) to increase the number of practitioners eligible to manage and/or prescribe appropriate medications. Medicare providers are uniquely positioned to create the gold standard of opioid use disorder treatment by screening, diagnosing, and treating Medicare patients for opioid use disorder as routine healthcare. They can also exhibit positive attitudes to reduce stigmas associated with opioid use disorder.
This session will consist of a panel discussion where, IPRO, the Quality Innovation Network-Quality Improvement Organization (QIN-QIO) will describe the state of the opioid crisis from a nursing home perspective and discuss how to improve patient safety in vulnerable populations. The Substance Abuse and Mental Health Services Administration (SAMHSA) will provide regulatory updates on opioid prescribing, the stigma of opioid addiction, and discuss key elements of Opioid Treatment Programs (OTPs). Finally, the Health Resources and Services Administration (HRSA), Federal Office of Rural Health Policy (FORHP), will share opioid-related resources and funding opportunities to engage partners in rural communities.
 April 8, 2024 17:00
April 8, 2024 17:00AI in Quality Measurements: Opportunities and Challenges in Health AI for a Resilient Health System

Brian Anderson, MD
CEO Coalition
for Health AI,
Inc.
This session will take a closer look at what the current state of clinical quality is in the US and the opportunities for AI to improve it, if implemented responsibly and effectively. CHAI is a community of health systems, public and private organizations, and expert practitioners of AI and data science, who have come together to harmonize standards and reporting for health AI and educate end-users on how to evaluate these technologies before adoption.
 April 8, 2024 17:30
April 8, 2024 17:30Closing Remarks

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services
 April 9, 2024 09:00
April 9, 2024 09:00Quality in Motion: Acting on the Centers for Medicare & Medicaid Services National Quality Strategy
Michelle Schreiber, MD
Deputy
Director,
Quality
& Value, Centers for Medicare & Medicaid Services

Susannah Bernheim, MD, MHS
Chief
Quality Officer
& Acting Chief Medical Officer,
Center for Medicare and Medicaid
Innovation,
Centers
for Medicare & Medicaid Services

Martin Hatlie, JD
Founding
Member,
Patients
for Patient Safety US

Jessica Lee, MD, MSHP
Acting
Chief Medical
Director,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services
In 2022, the Centers for Medicare & Medicaid Services (CMS) launched the CMS National Quality Strategy (NQS), a plan aimed at improving the quality and safety of health care for everyone, with a special focus on those from underserved and under-resourced communities. The CMS NQS builds on CMS’ efforts to improve health care quality for individuals across their lifespan and continuum of care by using all the Agency’s levers, including value-based payment programs and models; health and safety standards (including conditions for coverage and conditions of participation); survey and certification programs; quality measurement and public reporting; and quality improvement technical assistance. Join us to learn more about the recent publication, Quality in Motion: Acting on the CMS National Quality Strategy, and current CMS actions and accomplishments regarding equity and engagement, outcomes and alignment, safety and resiliency, and interoperability and scientific advancement.
 April 9, 2024 09:00
April 9, 2024 09:00Care for Complex Patients: Clinical Approaches to Quality Improvement at the Intersection Substance Use Disorder, Mental Illness, and Chronic Pain

Benjamin Springgate, MD, MPH, FACP
Professor of
Medicine and Public Health,
Louisiana State University Health-New
Orleans

Chinazo Cunningham
Commissioner,
New York State
Office of Addiction Services and Supports

Karran Phillips, MD, MSc
Deputy
Director,
Center for Substance Abuse Treatment,
SAMSHA

Stefan Kertesz, MD, MSc
Professor,
University
of Alabama at Birmingham Heersink School of Medicine and the Birmingham
Alabama Health Care System
Homeless PACT
This Mini Plenary will highlight expert clinicians’ and system leaders’ approaches to healthcare delivery and quality improvement for many of the most complex patients for whom American systems care – community members with comorbid substance use disorder, mental illness, and chronic pain. Patients with this complex triad often experience unmet healthcare needs and substantially worse health and social outcomes - reflecting not only clinical complexity but also significant challenges in accessing and paying for services, variations in quality of care, and entrenched system failures to address health related social needs. Leaders with deep clinical expertise and experience working in systems to improve care for people with substance use disorders, mental illness, and chronic pain will discuss their methods to tackle challenging clinical and social scenarios, recommending practical resources and that they and their systems use to integrate approaches to quality improvement, care delivery, and social determinants of health. Master Class experts will represent federal (SAMHSA Center for Substance Abuse and Treatment (invited)), clinical academic (the University of Alabama Birmingham and Department of Veterans Affairs (invited)), and state (New York Office of Addiction Services and Supports (invited)) systems, offering diverse vantage points and practical approaches and tools to address the needs of patients with this complex triad of conditions.
 April 9, 2024 10:30
April 9, 2024 10:30Welcome to Day 2 of the CMS Quality Conference

Jonathan Blum
Principal Deputy
Administrator &
Chief Operating Officer,
Office of the Administrator,
Centers for
Medicare & Medicaid
Services
 April 9, 2024 10:40
April 9, 2024 10:40CCSQ Priorities for 2024 and Beyond: Optimal Health for All People Across the Care Continuum

Anita Monteiro
Director, iQuality
Improvement &
Innovation Group
Centers for Medicare & Medicaid Services

Dora Hughes, MD, MPH
Acting
Chief Medical Officer
& Acting Director,
Center for Clinical Standards and Quality,
Centers for Medicare
& Medicaid Services

David Wright, MPA
Director,
Quality Safety
& Oversight Group,
Centers for Medicare & Medicaid
Services

Tamara Syrek Jensen
Director,
Coverage and
Analysis Group

Karen Tritz
Centers for Medicare
& Medicaid
Services
Director of the Survey & Operations Group
Michelle Schreiber, MD
Deputy
Director,
Quality & Value, Centers for Medicare & Medicaid Services

Lisa Parker
Centers for Medicare
& Medicaid
Services
Director of the Clinical Standard Group

Mark Plaugher
Centers for
Medicare & Medicaid
Services
Acting Director of the Information System Group (ISG)

Jennifer Dubbs
Director, Business
Operations
Group
Center for Clinical Standards and Quality
Centers for Medicare
and Medicaid
Services
 April 9, 2024 11:05
April 9, 2024 11:05Patient Safety Fireside Chat w/ CCSQ’s Acting Chief Medical Officer & Director and the Deputy Director of Quality and Value
Michelle Schreiber, MD
Deputy
Director,
Quality
& Value, Centers for Medicare & Medicaid Services

Dora Hughes, MD, MPH
Acting
Chief Medical Officer
& Acting Director,
Center for Clinical Standards and Quality,
Centers for Medicare
& Medicaid Services

Arjun Srinivasan, MD
Deputy
Director
Program
Improvement in the Division of Healthcare Quality Promotion at the Centers
for Disease Control and
Prevention (CDC)

Craig A. Umscheid, M.D., MS
Director,
Center
for Quality Improvement and Patient Safety (CQuIPS)
Agency for Healthcare
Research and Quality
(AHRQ)
Department of Health and Human Services
The Centers for Medicare & Medicaid Services (CMS) is committed to improving performance on key patient safety metrics through the application of CMS levers such as quality measurement, payment, health and safety standards, and quality improvement support. This session is a conversation with CMS Senior Leadership and Federal partners to renew our collective commitment to patient safety. We will be discussing progress that has been made, as well as challenges faced, since the 2023 CMS Quality Conference. Additionally, the panel will speak to a call to action for our healthcare community so that together we can achieve our patient safety goals.
 April 9, 2024 11:35
April 9, 2024 11:35Welcome Remarks from the Centers for Medicare and Medicaid Services Chief Dental Officer
Natalia Chalmers, DDS, MHSc, PhD
Chief Dental
Officer,
Office of the Administrator,
Centers for Medicare &
Medicaid Services
 April 9, 2024 11:45
April 9, 2024 11:45Remarks from HHS Inspector General Christi A. Grimm on Quality in HHS Programs

Christi A. Grimm
Inspector
General,
Office of
Inspector General,
Department of Health and Human Services
 April 9, 2024 13:30
April 9, 2024 13:30Advancing Multi-Payer Alignment and Specialty Care Integration through the Health Care Payment Learning and Action Network (LAN)

Kate Davidson LCSW
CMMI,
Centers for Medicare
& Medicaid Services,
Director of the Learning and Diffusion Group
(LDG)

Mark McClellan M.D., PhD
Director,
Margolis
Center for Health Policy at Duke University

Dr. Helen Burstin MD, MPH, MACP
CEO,
Council of
Medical Specialty Services
A critical part of advancing reform and addressing provider burden in the health care system is creating meaningful alignment among payers. Over the last year, both Center for Medicare and Medicaid Innovation (CMMI) and the Learning and Action Networks (LAN) have announced new models and initiatives meant to generate directional alignment that balances the need for multi-payer alignment goals with payer flexibility. This session describes how these efforts work together to generate this alignment at both the national and local levels.
Emphasizing both collaborative and individual efforts, CMMI and the LAN will highlight key initiatives and milestones generating meaningful multi-payer alignment across the healthcare market. In both instances, these efforts adopt the principles of directional alignment, where alignment does not require identical arrangements or programs, but looks to create collaboration and alignment around core areas, such as quality measurement, and create closer alignment over time.
Participants will learn how CMMI and the LAN are working together and with a wide range of partners to advance alignment in key areas of delivery system reform.
 April 9, 2024 13:30
April 9, 2024 13:30Improving Health Equity by Addressing Health-related Social Needs in Medicaid and CHIP

Jessica Lee, MD, MSHP
Acting
Chief Medical
Director,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services

Christopher Chen, MD, MBA, FACP
Medical
Director,
Medicaid Washington State Health Care Authority

Ruben Soliz, MPH
Federal
Relations Lead and Health
Policy Advisor
Arizona Health Care Cost Containment System
This session will explore recently released CMS guidance on health-related social needs (HRSN) and how states are implementing housing and nutritional supports to improve the quality of care and health outcomes. In November 2023, CMS issued an Informational Bulletin on how states can address health-related social needs (HRSN) in Medicaid and the Children’s Health Insurance Program (CHIP), and framework of services and supports considered allowable under specific authorities, including section 1115 demonstrations. CMS has approved 1115 demonstrations for HRSN services in states including Arizona and Washington. Presenters from these state Medicaid programs will describe how they have implemented housing and nutritional supports, integrating with existing social and housing services, as well as how they are measuring associated changes in health care utilization and quality, and health outcomes.
 April 9, 2024 13:30
April 9, 2024 13:30Working with Managed Care Plans to Improve Quality in Medicaid and CHIP:
Lessons from
the Infant
Well-Child Affinity Group

Emily Stauffer Rocha, MBA, MSN, RN, NE-BC, CHCQM,
Director of Clinical Innovation,
Texas Health and
Human Services
Commission

Crystal O'Reilly BSN, RN
AVP,
Quality and Care
Management Affairs,
Cook Children's Health Plan

Susan Ruiz, BA
EPSDT/Children’s
Health Subject
Matter Expert,
Division of Quality and Health Outcomes,
Children and
Adult Health Program
Group,
Center for Medicaid & CHIP Services
With more than 70% of Medicaid and Children's Health Insurance Program (CHIP)
beneficiaries enrolled in
managed care, states can have a significant impact on improving health services delivery
and outcomes
for their Medicaid and CHIP beneficiaries by working with their managed care plans
(MCPs) on quality
improvement (QI) initiatives. State staff from Texas Health and Human Services developed
an approach to
coordinating MCP QI efforts around a common state aim statement. Each MCP chose and
implemented an
improvement project to complement the state aim, and the state created a structure to
enhance peer
learning and impact. Participants will hear from a state speaker about their approach
and from a
participating MCP that ran its own supportive QI project. This session will also review
resources
developed by Centers for Medicare & Medicaid Services to help state Medicaid and
CHIP staff and
their MCP QI partners implement a similar approach.
 April 9, 2024 13:30
April 9, 2024 13:30Update on the Medicare Value-based Strategy
Michelle Schreiber, MD
Deputy
Director,
Quality & Value, Centers for Medicare & Medicaid Services

Purva Rawal, PhD
Chief Strategy
Officer at the CMS
Innovation Center
Centers for Medicare and Medicaid Services

John Pilotte
Director of the
Performance-based
Payment Policy Group (P3)
Center for Medicare at the Centers for
Medicare & Medicaid
Services
Sophia Sugumar (Moderator) MSHM
Program Policy
Lead,
Division of Electronic and Clinical Quality,
Centers for
Medicare & Medicaid
Services
The panel presentation will provide an update to the Medicare Value-Based Care Strategy. The presentation will specifically focus on progress along the three objectives of the Strategy—Alignment, Growth and Equity—as well as future priorities and vision.
 April 9, 2024 13:30
April 9, 2024 13:30Awareness to Action: Using a Structurally Competent Approach to Overcome Biases

Keith Norris MD
Distinguished
Professor of
Medicine,
UCLA Division of General Internal Medicine and Health Services
Research

Ken Teasley
Patient Facility
Representative
br/>NCC Legacy PSME
CAB, Harlem Wellness Center- MT. Sinai
Health disparities continue to persist among patients with End Stage Renal Disease (ESRD). Marginalized racial and ethnic minority and low socioeconomic populations have a disproportionate burden of involuntary discharges (IVDs) and other disparities, such as lack of access to transplantation and higher unplanned hospital readmissions. Structural competency for equitable kidney care is an approach in which healthcare professionals recognize and respond to health and illness as the downstream effects of broad social, political, and economic factors. It serves as an equity framework for overcoming disparities and bias in healthcare. Applying this approach in kidney care can play a significant role in reducing health disparities and advancing health equity. The ESRD National Coordinating Center (NCC) developed a three-module structural competency training for kidney professionals to address health inequities. The training provides specific, evidence-based interventions and strategies to address the structural drivers of kidney care inequities, including IVDs.
 April 9, 2024 13:30
April 9, 2024 13:30Optimizing Opioid Stewardship in 2024: How the Compass Program is Changing Clinical Care for Patients on Chronic Opioid Therapy

Jen Brockman, MHA, BSN, RN, CPPS,
Chief Clinical
Program Officer & OPSS Project Director,
Iowa Healthcare
Collaborative
Don Stader, MD, FACEP
OPSS
Medical Director &
Addiction Medicine Specialist,
Stader Opioid Consultants

Laurie Fisher, MD
Family
Medicine Physician &
OPSS Cohort,
Town Plaza Family Practice

Rachael Duncan, PharmD, BCPS, BCCCP
OPSS Coach,
Stader Opioid Consultants
This presentation will examine the implications of historical prescribing practices on patients receiving Chronic Opioid Therapy (COT) and assess the subsequent changes in prescribing patterns, patient access, and associated risks. This presentation will feature a panel from the Compass Program, including an addiction medicine physician, a pharmacist, a nurse, and a family medicine physician participant. The panel will discuss several of the core pillars of the Compass Program and how they are being implemented within the participant cohort to change clinical practice and improve patient outcomes. They will discuss resources to support opioid-sparing management of acute pain to reduce opioid exposure, utilizing nonopioid pharmacologic agents and nonpharmacologic therapies. For patients maintained on chronic opioid therapy (COT), the panel will discuss risk management strategies to increase patient safety including rotation to safer agents, providing naloxone, using patient-specific tapering strategies, and minimizing co-prescribing of other sedating agents. Lastly, the panel will discuss the critical need for primary care providers and family medicine physicians to help reduce overdose mortality trends by offering treatment of OUD with buprenorphine products, supported by resources, 1-on-1 coaching, and education from the Compass Program.
 April 9, 2024 13:30
April 9, 2024 13:30Who Seeks Medicare Support and Advocacy Services and How Can We Address Barriers and Reduce Disparities?

Scott Fortin, MBA
Sr. Director
Communications and
Outreach,
Kepro

Carmen Villegas, RN, BSN, BCPA
Immediate Advocacy
Manager,
Livanta

Stephanie Fry, BA, CPXP
Associate Vice
President,
Westat
In response to the President’s executive order to advance racial equity and support for underserved communities, the Department of Health and Human Services (HHS) established an equity action plan. In alignment with this plan, Beneficiary and Family-Centered Care Quality Improvement Organizations (BFCC-QIOs) are working to identify and address barriers to equitable access and utilization of beneficiary protection, support, and advocacy services.
BFCC-QIOs offer case review services for beneficiaries who think they may be entitled to additional Medicare-covered services, or who think the quality of care they received does not meet clinical standards. Using BFCC-QIO program data, we assessed the degree to which case review services are being utilized by beneficiaries of different races and ethnicities.
Disparities in case review utilization are evident among Hispanic and Asian beneficiaries and these disparities may further contribute to existing health outcome inequalities. The concern is that these beneficiaries are still experiencing premature healthcare service termination or other quality of care issues such as gaps between government and other health providers, but are not exercising their right to review and possibly resolve these issues through BFCC-QIO program services.
BFCC-QIOs are carefully analyzing the approach and implementation strategies for their work. Seeking input from experts, stakeholders and Medicare beneficiaries, BFCC-QIOs are identifying strategies to improve access and awareness and reduce disparities in use of BFCC-QIO case review services that may contribute to poor health outcomes.
 April 9, 2024 13:30
April 9, 2024 13:30Expanding Access to Quality and Affordable Oral Health and Behavioral Healthcare

Jessica Maksut PhD
Technical
Director,
Office
of Minority Health;
Centers for Medicare & Medicaid Services

Carla Shoff PhD,
Senior Advisor
to the Chief
Dental Officer,
Office of the Administrator;
Centers for Medicare
& Medicaid
Services

Lorel Burns DDS, MS
Assistant
Professor,
NYU
College of Dentistry
Over the past two years, CMS has made significant strides in advancing oral health across all our programs. CMS has developed a set of cross-cutting initiatives that engage teams across our organization to drive the goals highlighted by the strategic pillars and enhance focus on critical components of our work. These initiatives are high-level, multi-year priorities for CMS that bring our centers and offices together to leverage their expertise and strengthen collaboration. The CMS Chief Dental Officer will describe the launch and work under the Oral Health Cross-Cutting Initiative. Access to oral health services promotes health and wellness and allows beneficiaries and consumers to achieve the best health possible. States have the flexibility to determine what dental benefits are provided to adult Medicaid enrollees. While most states offer at least emergency dental services for adults, less than half of the states currently provide comprehensive dental care. There are no minimum requirements for adult dental coverage. More than 1 in 4 (26%) adults in the United States have untreated tooth decay. Over the last ten years, dental pain has been a top reason for opioid prescribing upon discharge from the ED, thereby contributing to the overdose crisis. There is a bi-directional link between oral health and substance use disorder. This session will focus on the outcomes of two studies that analyzed Medicaid enrollment and claims data. These studies examine oral health needs, disparities, and access to dental services for Medicaid adults with substance use disorders, as well as the impact of the COVID-19 public health emergency, state coverage policies, and socio-demographic factors on adults' access to dental services.
 April 9, 2024 13:30
April 9, 2024 13:30Lessons from Human Centered Design Informing Policymaking: Substance Use Disorders and Oral Health

Morgan Taylor
Lead Human Center
Design
Specialist,
Office of Burden Reduction & Health Informatics
(OBRHI)
The Customer Focused Research Group (CFRG) within the Office of Burden Reduction and Health Informatics (OBRHI) will present on their Behavioral Health and Oral Health Human-Centered Design Customer Engagements. Human-Centered Design (HCD) is the process CMS uses to understand the people for which they write policies; and create programs and services. CFRG will share the qualitative research aimed at understanding how to ensure equitable access to oral health care without stigma. Each respective engagement revealed many insights in addition to an opportunity to co-create illustrations with external customers to highlight and raise the customers’ voice in supporting those suffering with substance use disorders.
 April 9, 2024 13:30
April 9, 2024 13:30The 2024 National Impact Assessment Report – Collecting and Using Quality Data Across 26 CMS Programs

Robert Ziemba, PhD
Statistician,
HSAG

Kyle Campbell, PharmD
Project
Director,
HSAG

Kendra Hanley, MS, BA
Impact
Assessment Team
Lead,
HSAG
The 2024 National Impact Assessment aggregates retrospective data from 26 CMS quality and value-based incentive programs to characterize quality and efficiency impacts associated with the use of measures. The session will focus on summarizing key findings from these comprehensive analyses that provide important insights regarding effects of the COVID-19 pandemic during the period of analysis. We will describe national measure performance trend data pre-COVID-19 (2016–2019) compared with results in the initial years of the COVID-19 public health emergency (PHE)— 2020 and 2021— and describe patient impact and costs avoided when performance for select measures improved. Data also will be presented on how the CMS measure portfolio is evolving to reduce measurement burden and address CMS quality priorities. Lessons learned from the COVID-19 PHE and proposed actions to improve the resilience of quality measurement and the health care system will be discussed. Finally, underscoring equity as a primary objective of the CMS National Quality Strategy, the session will explore patterns of disparities in quality measure scores and offer insight into underlying drivers of disparities identified through focus groups in underserved communities.
 April 9, 2024 13:30
April 9, 2024 13:30Breaking Barriers: Enhancing Language Access in Health and Human Services

Maria Moreno MPH
Program Manager
Sutter Health

Genevieve Babecki
Language
Access Coordinator,
HHS/Office of Civil Rights

Lina Rashid
Senior Policy
Advisor,
Centers for
Medicare and Medicaid Service/Center for Consumer Information and Insurance
Oversight

Anita Pinder
Director,
Centers for Medicare
& Medicaid Services/Office of Equal Opportunity & Civil
Rights
Approximately 68 million people in the United States speak a language other than English at home, and of those, 8.2% speak English less than very well. Individuals with limited English proficiency (LEP) do not speak English as their preferred language and have a limited ability to read, write, speak, or understand English. A lack of meaningful language access can lead to inequitable access to health and human services. Research indicates that adverse events affect patients with LEP more frequently, are often caused by communication problems, and are more likely to result in serious harm compared to those that affect English-speaking patients. Providing language access decreases barriers to equal access to health and human services. During this session, you will hear from three leaders working to ensure language access. They will share insights from the federal perspective with a focus on policy and communications, as well as from one large health system and their 20-year experience with language services.
 April 9, 2024 13:30
April 9, 2024 13:30Innovation Center Quality Pathway – A Refreshed Approach to Quality in CMMI Models

Susannah Bernheim, MD, MHS
Chief
Quality Officer
& Acting Chief Medical Officer,
Center for Medicare and Medicaid
Innovation,
Centers
for Medicare & Medicaid Services
Noemi Rudolph, MPH
Director,
Research and
Rapid Cycle Evaluation Group,
Center for Medicare and Medicaid
Innovation (CMMI)

Jacob Quinton, MD, MPH
Medical
Officer,
Center
for Medicare and Medicaid Innovation (CMMI),
Centers for Medicare &
Medicaid
Services
The purpose of the proposed panel is to describe the Centers for Medicare & Medicaid Services Innovation Center’s approach to strengthening the focus on quality, outcomes, and experience within the Innovation Center’s alternative payment models. The resulting Quality Pathway emerged from the 2021 strategic refresh and includes development of a process to certify models for expansion based on quality improvement. The panel will introduce the pathway, describing how it elevates patient outcomes and experience of care within alternative payment models and emphasizes the translation of a model’s theory of action into measurable benefits for patients. The panel will discuss how this alignment of model design and quality strategy also drives new approaches to model evaluation, and how the Quality Pathway will be used to identify when a model may be eligible for expansion based on demonstrated quality improvement in alignment with CMMI’s statutory mandate.
Having addressed the conceptual basis for the Pathway, the panel will share examples of models recently under development to demonstrate how the pathway will be used at the Center. This will include insight into design choices around measure selection, implementation decisions on data collection, and evaluation considerations on methodological approach. As part of discussing implementation of the pathway, the panel will identify a number of considerations entailed in executing this new approach to model quality strategies at the Center, such as those associated with novel measure development and rigorously evaluating the impact of models on patient outcome and experience.
 April 9, 2024 13:30
April 9, 2024 13:30Advancing Oral Health Equity Through Quality Improvement Measures

Meagan Khau, MHA (Moderator)
Director,
Data
and Policy Analytics Group,
Office of Minority Health,
Centers for
Medicare & Medicaid
Services

Kimia Imani, MS
DDS/PhD
Student,
University of
Washington School of Dentistry

Kaylie Magidson, DDS
Pediatric
Postdoctorate
Student,
New York University College of Dentistry

Beau Meyer, DDS, MPH
Associate
Professor,
The
Ohio State University College of Dentistry
Oral health is a crucial component of overall well-being. States are mandated to provide dental care for children under Medicaid and the Children's Health Insurance Program (CHIP). However, a 2023 report revealed that only 46% of Medicaid-insured children and teens had a dental check-up in 2018. The COVID-19 pandemic further hindered access to dental services, with a 20% reduction in treatments for children. This decrease in access to preventive and necessary dental care has led to a higher reliance on emergency services and the need for antibiotics to treat advanced dental issues and their complications. The pandemic also necessitated a shift towards less invasive treatments, like silver diamine fluoride (SDF). Healthcare systems aiming to enhance patient experience often encounter significant obstacles, indicating the necessity to modify behaviors and practices throughout various organizational levels and sectors. However, they can also benefit from applying well-established principles and methods for quality improvement (QI).
This session will delve into the findings from three joint studies analyzing enrollment and claims data from the Transformed Medicaid Statistical Information System (T-MSIS). These studies aim to understand how Medicaid-enrolled children used oral health services during 2019, 2020, and 2021. The data reveals patterns over time and highlights significant variations based on geography and demographics. Notably, there has been no substantial change in the rates and duration of antibiotic prescriptions for dental issues. Nevertheless, there is a marked increase in the use of silver diamine fluoride and a growing number of emergency department visits for non-traumatic dental problems, especially among children with special healthcare needs. These trends highlight numerous opportunities for quality improvement efforts at various levels and areas within the dental care system.
 April 9, 2024 13:30
April 9, 2024 13:30Telehealth: Improving Access to Care for Tribes: CMS and IHS Updates

Susan Karol, MD
Chief Medical
Officer,
Division of Tribal Affairs,
Centers for Medicare & Medicaid
Services

Susy Postal, DNP, RN-BC
Chief
Informatics
Officer,
Indian Health Service
Chris Fore, PhD
Director,
Indian Health
Service Telebehavioral Health Center of Excellence
The Indian Health Service (IHS) continues to support the expanded use of telehealth to provide patient care after the COVID-19 Public Health Emergency (PHE). This presentation will focus on an overview of the use of telehealth at the IHS and the support the Centers for Medicare & Medicaid Services (CMS) provides. The presentation will include the accomplishments in expanding telehealth from April 2020 to the present. The various telehealth services available at the IHS will be discussed including CMS’s support provided to rural and frontier areas. Issues in providing audio-only services will be discussed and aligned with services on the Medicare Telehealth Services List for CY 2024. Presenters will provide metrics describing the utilization of telehealth in IHS. Telehealth best practices will be discussed, and quantitative and qualitative results from IHS patient and IHS provider telehealth surveys will be addressed. Finally, patient outcomes utilizing telehealth services will be included and quality improvement options provided.
 April 9, 2024 14:30
April 9, 2024 14:30Improving Outcomes in Organ Donation and Transplantation: The Organ Transplant Affinity Group (OTAG) Action Plan

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services

Suma Nair, PhD, MS, RD
Associate
Administrator,
Health Services Bureau,
Health Resources and Services
Administration
There is no denying that that there is much work to be done to improve the transplantation system as there are over 100, 000 patients waiting for organ transplants, as of October 2023.
In September 2023, a federal collaborative, led by the Centers for Medicare & Medicaid Services (CMS) and the Health Resources and Services Administration (HRSA), called the Organ Transplantation Affinity Group (OTAG), launched with a goal of strengthening accountability, equity, and performance to improve access to organ donation, procurement, and transplantation for patients, donors, families and caregivers, and providers.
Join this listening session to learn about and provide feedback on OTAG’s mission to strengthen federal oversight and support of the organ transplantation system.
 April 9, 2024 14:30
April 9, 2024 14:30The Age-Friendly Health Systems Movement: How Focusing on Quality and Safety for Older Patients Builds Resilience

Terry Fulmer, PhD, RN, FAAN
President,
The
John A. Hartford Foundation

Leslie Pelton, MPA
Vice
President,
Institute
for Healthcare Improvement
Learn about the Age-Friendly Health Systems movement and how it leads to improved outcomes for older adults and health system resilience. Presenters will share actionable opportunities, implementation successes and programs for specific settings.
 April 9, 2024 14:30
April 9, 2024 14:30Healthcare and Public Health Cyber Security: Keeping Patients Safe and Secure

Brian Mazanec, PhD
Deputy
Director,
Office of
Preparedness,
Department of Health and Human Services
The Healthcare and Public Health (HPH) sector continues to experience increasingly sophisticated cyberattacks that exploit complex hospital infrastructures, underfunded cybersecurity functions, and numerous vulnerable legacy medical devices. These cyberattacks against the sector are growing both in numbers and severity. ASPR, in its Sector Risk Management Agency (SRMA) role and with active involvement from stakeholders across the Department of Health and Human Services (HHS), proactively confronts these growing cyber threats and strengthens the HPH sector’s cybersecurity posture. In December, HHS published a roadmap outlining how the department will level up to this challenge to make our healthcare system more resilient and prepared for cyber threats. In January, aligned with the first pillar in this new roadmap, HHS—through ASPR—published HPH Cybersecurity Performance Goals to further help healthcare organizations implement these high-impact cybersecurity practices.
 April 9, 2024 14:30
April 9, 2024 14:30Improving Healthcare Quality: Beginning with the End in Mind

Anita Monteiro
Director, iQuality
Improvement &
Innovation Group
Centers for Medicare & Medicaid Services
Timmy T. Nelson
Patient
Advocate/Outreach Advisor,
UPS (retired)/Network 4, Quality Insights,
Chester County Community
Foundation

Sven T. Berg, MD, MPH
Chief
Executive Officer,
Quality Insights
Data-driven quality improvement is the foundation of healthcare transformation. The ability to visualize the end goals, outcomes and results, strategically leverage healthcare data, then design a quality improvement process/intervention to deliver outcomes is what separates the highly effective quality improvement professionals from those that are not. This session focuses on the practices and interventions quality improvement professionals can use on a daily basis to help them relate the small decisions to the bigger picture and ensure that what’s produced eventually will be valuable.
 April 9, 2024 15:30
April 9, 2024 15:30Advancing Oral Health Equity Through Quality Improvement Measures

Meagan Khau, MHA (Moderator)
Director,
Data
and Policy Analytics Group,
Office of Minority Health,
Centers for
Medicare & Medicaid
Services

Kimia Imani, MS
DDS/PhD
Student,
University of
Washington School of Dentistry

Kaylie Magidson, DDS
Pediatric
Postdoctorate
Student,
New York University College of Dentistry

Beau Meyer, DDS, MPH
Associate
Professor,
The
Ohio State University College of Dentistry
Oral health is a crucial component of overall well-being. States are mandated to provide dental care for children under Medicaid and the Children's Health Insurance Program (CHIP). However, a 2023 report revealed that only 46% of Medicaid-insured children and teens had a dental check-up in 2018. The COVID-19 pandemic further hindered access to dental services, with a 20% reduction in treatments for children. This decrease in access to preventive and necessary dental care has led to a higher reliance on emergency services and the need for antibiotics to treat advanced dental issues and their complications. The pandemic also necessitated a shift towards less invasive treatments, like silver diamine fluoride (SDF). Healthcare systems aiming to enhance patient experience often encounter significant obstacles, indicating the necessity to modify behaviors and practices throughout various organizational levels and sectors. However, they can also benefit from applying well-established principles and methods for quality improvement (QI).
This session will delve into the findings from three joint studies analyzing enrollment and claims data from the Transformed Medicaid Statistical Information System (T-MSIS). These studies aim to understand how Medicaid-enrolled children used oral health services during 2019, 2020, and 2021. The data reveals patterns over time and highlights significant variations based on geography and demographics. Notably, there has been no substantial change in the rates and duration of antibiotic prescriptions for dental issues. Nevertheless, there is a marked increase in the use of silver diamine fluoride and a growing number of emergency department visits for non-traumatic dental problems, especially among children with special healthcare needs. These trends highlight numerous opportunities for quality improvement efforts at various levels and areas within the dental care system.
 April 9, 2024 15:30
April 9, 2024 15:30HHS’ Call to Action on Opioid Use Disorder Treatment

Robert Accetta, RPh, BCGP, FASCP
Senior
Pharmacist,
IPRO QIN_QIO

Megan Meacham, MPH
Director,
Rural Strategic
Initiatives Division,
Health Resources and Services Administration
(HRSA)

Wanda Pamphile, PharmD, MPH
Senior Health Insurance
Specialist,
Centers for Medicare & Medicaid Services

Karran Phillips, MD, MSc
Deputy
Director,
Center for Substance Abuse Treatment,
SAMSHA
Drug overdose deaths in the United States, driven by illicit fentanyl and other opioids, remain at historically high levels – with more than 107,000 lives lost in the past year, and millions more struggle with opioid and other substance use disorders. The opioid crisis reaches every corner of our country, from alleyways to nursing homes, and requires an immediate call to action. Federal partners, local governments, healthcare institutions, and communities are working together to provide viable solutions to combating the opioid crisis.
There is a nationwide need for education on medications for opioid use disorder (MOUD) to increase the number of practitioners eligible to manage and/or prescribe appropriate medications. Medicare providers are uniquely positioned to create the gold standard of opioid use disorder treatment by screening, diagnosing, and treating Medicare patients for opioid use disorder as routine healthcare. They can also exhibit positive attitudes to reduce stigmas associated with opioid use disorder.
This session will consist of a panel discussion where, IPRO, the Quality Innovation Network-Quality Improvement Organization (QIN-QIO) will describe the state of the opioid crisis from a nursing home perspective and discuss how to improve patient safety in vulnerable populations. The Substance Abuse and Mental Health Services Administration (SAMHSA) will provide regulatory updates on opioid prescribing, the stigma of opioid addiction, and discuss key elements of Opioid Treatment Programs (OTPs). Finally, the Health Resources and Services Administration (HRSA), Federal Office of Rural Health Policy (FORHP), will share opioid-related resources and funding opportunities to engage partners in rural communities.
 April 9, 2024 15:30
April 9, 2024 15:30Using School-based Services to Improve Behavioral Health Service Delivery to Children in Medicaid and CHIP

Kate Ginnis MSW, MPH
CMCS Senior
Advisor for Youth
Coverage
Centers for Medicare and Medicaid Service
Medicare &
Medicaid Services

Kate Yager MA
Director of
Medicaid
Chicago
Public Schools

Sergio Obregón M.Ed.
Bureau Chief
for Medical
Eligibility and Special Programs, Division of Eligibility
Illinois
Department of Healthcare and
Family Services
It is a focus of the Biden-Harris Administration to make it easier for states to support schools in providing critical health care services, especially mental health services, for millions of students across the nation. The Bipartisan Safer Communities Act helped pave the way for the Medicaid guidance Delivering Services in School-Based Settings: A Comprehensive Guide to Medicaid Services and Administrative Claiming announced in May 2023 as a significant overhaul of school Medicaid billing. The new guidance is designed to streamline the process of school-based billing and increase students’ access to healthcare at school. This session provides an overview of the flexibilities provided in the guide, including allowing state Medicaid agencies to change the way that services are paid for in schools, as well as which providers can bill for services in schools. This session will highlight intra-state coordination between a State Medicaid Agency and Local Educational Agency (LEA) to leverage school-based services to improve behavioral health service delivery to children in Medicaid and CHIP and how they are measuring the improvements (e.g., increasing claiming and delivery of behavioral health services). This session will highlight how states can ease the administrative burden for schools so that more services can be paid for by Medicaid/CHIP—bringing more money into the schools for health services—and by extension allowing for more services.
 April 9, 2024 15:30
April 9, 2024 15:30Building Capacity to Improve HIV Viral Suppression Data Among Medicaid Beneficiaries

Bashirat Olayanju, MPH,
Director,
Health System
NASTADs Integration

Marlene Matosky MPH, RN,
Chief -
Clinical and
Quality Branch
Health Resources and Services
Administration

Parker James, MPP,
Policy Analyst
The Hilltop
Institute
The HIV viral suppression measure included in CMS’ Adult Core Set (HVL-AD) offers a unique opportunity to promote inter-program, intra-state collaboration to share data and develop joint and/or complementary policies to drive high-impact, sustainable improvement for Medicaid beneficiaries living with HIV. NASTAD was funded by the Health Resources and Services Administration (HRSA) HIV/AIDS Bureau (HAB) to support building the capacity to calculate and report the HVL-AD measure to CMS, through the implementation of a quality improvement collaborative. Calculation of the HVL-AD measure uniquely utilizes multiple data sources in addition to claims data, including clinical and laboratory data received by public health programs. Panelists for this session will discuss how the use of multiple data sources across both Medicaid and public health programs, served as the catalyst for inter-agency collaboration, in which they will focus on recent experiences initiating HVL-AD reporting and use the data from a participating state in the collaborative. Panelists will highlight the process of inter-agency engagement, their team accomplishments and lessons learned particularly highlighting collaboration strategies. The session will offer insights into what it takes to create the conditions for both enabling collaboration as well as how that collaboration has led to the strategic use of the data plan engagement strategies that will support the improvement of health outcomes for Medicaid beneficiaries living with HIV.
 April 9, 2024 15:30
April 9, 2024 15:30Aligning Quality Measures and Program: The CMS National Quality Strategy in Action

Jessica Lee, MD, MSHP
Acting
Chief Medical
Director,
Center for Medicaid and CHIP Services,
Centers for
Medicare & Medicaid
Services

Douglas Jacobs, MD, MPH
Chief
Transformation Office
Center for Medicaid and CHIP Services;
Centers for Medicare &
Medicaid
Services

Susannah Bernheim, MD, MHS
Chief
Quality Officer
& Acting Chief Medical Officer,
Center for Medicare and Medicaid
Innovation,
Centers
for Medicare & Medicaid Services
Michelle Schreiber, MD
Deputy
Director,
Quality & Value, Centers for Medicare & Medicaid Services
Increasing alignment and coordination across CMS quality programs and initiatives focuses
our attention
on high priority clinical areas and amplifies the impact of CMS actions. The CMS
National Quality
Strategy serves as a guide for collaboration as we concentrate our efforts to advance
health equity,
address maternal morbidity and mortality, streamline the CMS quality measurement
portfolio, and improve
the delivery of safe care. Join us to hear the current activities and accomplishments of
programs across
CMS as we work to get closer to the high-quality, safe, equitable, and resilient health
care system
envisioned for all individuals.
 April 9, 2024 15:30
April 9, 2024 15:30Million Hearts 2027: Aiming for Impact with a Focus on Health Equity

Haley Stolp
Policy and
Partnership Strategist,
Centers for Disease Control Disease Control and Prevention
Laurence Sperling, MD, FACC, FAHA, FACP, FASPC
Executive Director,
Million Hearts Initiative,
Centers for Disease
Control and
Prevention

Taylor Streeter, MPH
Health
Scientist,
ASRT,
Inc.
Million Hearts® prioritized strategies for building healthy communities and optimizing care through a committed focus on specific populations experiencing inequities. This session describes how Million Hearts 2027 is addressing health equity with a review of communication assets and opportunities for engagement, an exploration of health equity-related issues for widespread use of self-measured blood pressure monitoring and cardiac rehabilitation, and an overview of new and future opportunities to reduce cardiovascular maternal health disparities.
 April 9, 2024 15:30
April 9, 2024 15:30Bridging the Gaps in the Kidney Transplant Journey: New Collaboration in CKD

Victoria Cash MBA, BSN, RN, CPHQ
Executive
Director,
IPRO ESRD Network of the Ohio River Valley

Ivory Harding, MS
Director,
Quality and
Regulatory Affairs,
National Kidney Foundation

Matthew Cooper MD
Chief of
Transplantation,
Director of the Solid Organ Transplant Line and Professor of Surgery at the
Medical College of
Wisconsin,
Medical College of Wisconsin

Patrick Gee Ph.D
Founder,
iAdvocate

Sherri Morgan-Johnson RN, BSN, MHSA, FAC-COR III
Nurse Consultant,
Centers for Medicare &
Medicaid Services

Sumeska Thavarajah, MD
Medical
Director,
Fresenius Kidney Care
During this patient-centered roundtable session, attendees will learn from kidney dialysis/transplant patients, the NKF, ESRD Networks, QIN-QIOs, TAQIL, and experts as they explore the complete kidney transplant journey.
From the five CKD stages to dialysis treatment options, and the transplant process, the expert panel will highlight gaps throughout the transplant care continuum and identify potential solutions, including strategies to reduce inequities experienced by underserved communities.
To address these identified gaps, speakers will review available partnership opportunities, new programs being tested in select communities, critical resources accessible to healthcare professionals, as well as the vital need to improve patient education that is culturally and linguistically appropriate throughout the kidney care system.
 April 9, 2024 15:30
April 9, 2024 15:30Supporting Equity at Scale Across HQIC-enrolled Hospitals

Laura Benzel, MS, BS, CCSGB,
Project Director,
Health Equity Lead,
IPRO

Natalie Graves MPH,
Director,
Research &
Implementation,
Convergence Health Consulting

Nicole Ford MBA, CPHQ,
Project
Manager,
Healthcare Association of New York State

Rosa Abraha MPH,
Health Equity
Lead,
Alliant
Health Solutions
IPRO and Alliant Health Solutions deployed multiple assessments and conducted technical assistance to understand the current health equity needs of Hospital Quality Improvement Contractors (HQIC) supported hospitals. The responses revealed that hospitals are most concerned about and need support for preparing for the new CMS health equity reporting requirements. In response, IPRO and Alliant Health Solutions developed multiprong approaches to support hospital health equity implementation, including Learning and Action Networks (LAN) with subject matters experts, affinity groups, one-on-one technical assistance, SDOH resources, discharge tools, a dynamic six-step model for hospital health equity implementation, and a bite-sized learning video series on health literacy, cultural and linguistically appropriate standards (CLAS). Additionally, Alliant Health Solutions worked with a hospital in Georgia, which prompted dedicated monthly health equity office hours co-led by the Alliant Health Solutions health equity lead and a representative from the Georgia hospital.
In addition, the HANYS and Convergence HQIC teams will describe organizational approaches to addressing and advancing health equity. HANYS will describe their experience developing and administering a health equity gap analysis assessment and how hospitals have used the tool, identified gaps, and taken action by addressing & implementing practice recommendations across all 7 assessment categories. The Convergence HQIC team will describe the approach to equity that focuses on building reliable, culturally sensitive processes for implementing a Social Drivers of Health (SDOH) screening program in hospitals across a variety of settings.
 April 9, 2024 15:30
April 9, 2024 15:30Medicare Beneficiaries Hospital Readmissions: Prevention and Cost Evaluation

Stephanie Hursey, MSN, MHA, CCM (Moderator),
Contract Officer Representative,
Centers for
Medicare & Medicaid
Services, DCPH

Vanessa Andow, CPHQ, CPPS, FACHE,
Project Director,
TMF Health Quality Institute

Sadiq Bouda Abdulai, PhD
Senior
Data Analyst,
Quality Insights

Jill Manna BA, PMP.
Quality
Improvement Specialist,
TMF Health Quality Institute

Grace Bolanos Sewell, MA, CCLS, CPHQ
Quality
Improvement Specialist,
TMF Health Quality Institute
Attend this presentation to hear about the work Quality Insights and TMF Health Quality Institute, two Quality Innovation Network-Quality Improvement Organizations, have done around hospital readmissions.
The first part of this session will focus on how standardization of communication can reduce or prevent unnecessary hospital readmissions across the continuum of care. Since 2019, the TMF Quality Innovation Network-Quality Improvement Organization healthcare quality improvement specialists, along with health care providers and partners in the community of El Paso, Texas, identified poor communication among the health care providers in the community that resulted in high readmission rates. To combat these rates, the community developed a Nurse-to-Nurse Report to standardize communication among the health care providers in the community that treat the same patients being readmitted.
The second part of this session will compare parametric and nonparametric cost estimates for hospital readmissions. Using Medicare claims data from Pennsylvania and West Virginia spanning 2017-2022, we estimate how much more, on average, Medicare beneficiaries with selected index diagnoses cost when readmitted within 30 days, compared to those not readmitted, after controlling for demographics and comorbidities. This estimation is accomplished via a robust machine learning variable importance framework. This approach avoids the assumptions associated with parametric methods, and thus enhances accurate valuation."""
 April 9, 2024 15:30
April 9, 2024 15:30Infusing Technology and Innovation to Reduce Burden and Improve Services for Medicare Beneficiaries

Wendy Gary, MHA, (Moderator)
Chief Operating
Officer,
Avar Consulting;
Executive Director,
BFCC-QIO;
Project Director,
BFCC
NCORC

Josh Dominick, MPA,
Director,
Business Intelligence
Kepro

Jed Shakarji,
Data Analyst II,
Avar
Consulting

Brian Salzer, MS, PMP
Data
Science Team Lead,
Avar Consulting
Rapidly advancing technology, access to data, and secure ways to communicate with an increasingly tech-savvy cross-section of the American population has changed how we think about protecting Medicare beneficiaries and the Medicare Trust Fund. Beneficiary and Family-Centered Care Quality Improvement Organizations (BFCC-QIOs) are adopting strategies to improve access and efficiency while reducing burden for all parties.
In their scope of improving the effectiveness, efficiency, economy and quality of services provided to Medicare beneficiaries, BFCC-QIOs review case documentation, medical records, and/or Medicare claims for more than 400,000 records annually. BFCC-QIOs also produce detailed documentation for providers and Medicare beneficiaries to summarize findings for beneficiary-initiated quality of care reviews. Continuously looking to improve quality, BFCC-QIOs identified ways to streamline processes, resulting in improved outcomes and beneficiary- and family-centered services.
To support providers, BFCC-QIOs are implementing cutting edge technologies such as artificial intelligence and machine learning to create efficiencies in case review and documentation processes; these have resulted in reduced burden, improved patient-safety and improved standardization. To support beneficiaries, BFCC-QIOs utilize these tools to ensure appropriate implementation of plain language in documentation intended for beneficiaries and families. Finally, to support the Medicare Trust fund, BFCC-QIOs developed approaches to streamline records review and more efficiently use physician review time for identification of cases that are likely to be misaligned with CMS policies.
While technology cannot replace the need for human review, input, and interactions, BFCC-QIOs have identified ways to maximize efficiencies and use administrative, clinician, and beneficiary time when it is most valuable.
 April 9, 2024 15:30
April 9, 2024 15:30Expanded Access to Quality and Affordable Oral Health and Behavioral Healthcare

Jessica Maksut PhD
Technical
Director,
Office
of Minority Health;
Centers for Medicare & Medicaid Services

Carla Shoff PhD,
Senior Advisor
to the Chief
Dental Officer,
Office of the Administrator;
Centers for Medicare
& Medicaid
Services

Lorel Burns DDS, MS
Assistant
Professor,
NYU
College of Dentistry
Natalia Chalmers, DDS, MHSc, PhD
Chief Dental
Officer,
Office of the Administrator,
Centers for Medicare &
Medicaid Services
Over the past two years, CMS has made significant strides in advancing oral health across all our programs. CMS has developed a set of cross-cutting initiatives that engage teams across our organization to drive the goals highlighted by the strategic pillars and enhance focus on critical components of our work. These initiatives are high-level, multi-year priorities for CMS that bring our centers and offices together to leverage their expertise and strengthen collaboration. The CMS Chief Dental Officer will describe the launch and work under the Oral Health Cross-Cutting Initiative. Access to oral health services promotes health and wellness and allows beneficiaries and consumers to achieve the best health possible. States have the flexibility to determine what dental benefits are provided to adult Medicaid enrollees. While most states offer at least emergency dental services for adults, less than half of the states currently provide comprehensive dental care. There are no minimum requirements for adult dental coverage. More than 1 in 4 (26%) adults in the United States have untreated tooth decay. Over the last ten years, dental pain has been a top reason for opioid prescribing upon discharge from the ED, thereby contributing to the overdose crisis. There is a bi-directional link between oral health and substance use disorder. This session will focus on the outcomes of two studies that analyzed Medicaid enrollment and claims data. These studies examine oral health needs, disparities, and access to dental services for Medicaid adults with substance use disorders, as well as the impact of the COVID-19 public health emergency, state coverage policies, and socio-demographic factors on adults' access to dental services.
 April 9, 2024 15:30
April 9, 2024 15:30The True Cost of Patient Safety Events and Pursuing the Goal of Zero Harm
Li Chen, Ph.D
Health Research
Lead,
Avar
Consulting

Jacklyn Vollmer, MPH
Quality
Improvement and
Operations Support Specialist,
Avar Consulting
Patient safety events (PSEs) remain a persistent challenge in our healthcare system, and the Centers for Medicare & Medicaid Services (Centers for Medicare & Medicaid Services) has adopted the goal of Zero Preventable Harm as part of its National Quality Strategy (NQS). This presentation will (1) discuss the prevalence of PSEs among Medicare beneficiaries, (2) analyze associated additional inpatient care and financial costs, and (3) provide insight to support Centers for Medicare & Medicaid Services’ aim to promote the safest possible care for all. The Beneficiary and Family Centered Care National Coordinating Oversight and Review Center (BFCC NCORC) screens 4,000 Medicare medical records annually for PSEs, leading to follow-up actions by the BFCC-Quality Improvement Organizations (QIOs). NCORC analyzed additional days of hospitalization and payment associated with PSEs projected on a national level, by sample weighting, representing beneficiaries based on 4,000 Medicare discharges between October 2020 and December 2021. Over 5,000 PSEs were identified, and half of beneficiaries experienced at least one, with 6% being deemed preventable. PSEs were associated with nearly four additional days of inpatient care on average, totaling 32.5 million additional days nationally. This equates to $86 billion per year, or about one-tenth of all Medicare spending. Preventable PSEs cause about 5.7 million additional days of care, and over $15 billion in spending. Patient safety is the cornerstone of high-quality healthcare, yet PSEs happened in more than half of Medicare beneficiary hospitalizations, accounting for nearly 10% of all Medicare spending. These findings reinforce the urgent need for Centers for Medicare & Medicaid Services’ quality agenda, and the goal of achieving zero preventable harm.
 April 9, 2024 16:30
April 9, 2024 16:30Chartering the Course to Zero Harm

Tejal Gandhi, MD, MPH, CPPS
Chief Safety and
Transformation Officer,
Press Ganey
This session will explore the broader definition of harm beyond physical safety, and the importance of addressing inequities to achieve zero harm. Dr. Gandhi will share strategies and tactics to show how leading organizations are innovating and transforming a culture and leveraging high reliability to build engaged, resilient care teams that deliver safe, high-quality care and the optimal patient experience.
 April 9, 2024 17:00
April 9, 2024 17:00Closing Remarks

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services
 April 10, 2024 10:00
April 10, 2024 10:00Welcome

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services
 April 10, 2024 10:05
April 10, 2024 10:05Lessons Learned from the Forefront: Resident Socialization, Staffing Stabilization, and Facility Support

Lenise Cummings-Vaughn, MD, CMD
Medical
Officer,
Center for Clinical Standards and Quality,
Centers for
Medicare & Medicaid
Services
As the newest Medical Officer to join CMS, Dr. Lenise Cummings-Vaughn will share her insights and lessons learned as a Hub leader for the AHRQ ECHO National Nursing Home COVID Action Network and the themes that emerge including balancing patient needs for socialization with infection control, resource management, staffing stabilization, burn out, and education on best practices and quality assessment and improvement.
 April 10, 2024 10:30
April 10, 2024 10:30The Moving Forward Coalition Promotes Strengthening Resident Councils
Anna Fisher, CADDCT, CDP, CMDCP, CDSGF, QCP
Education Consultant/Nurse,
Hillcrest Health
Services

Mairead Painter, BSW
Long Term
Care Ombudsman,
State of Connecticut
This session will demonstrate how one of the committees that is part of the Moving Forward Coalition assembled residents, care partners, advocates, and researchers to develop a step-by-step Resident Council Guide for nursing home residents, staff, and community members. We will describe how the guide is currently being piloted and tested in 4 nursing homes and what we hope to learn from this pilot. We will discuss the importance of a resource guide and its use to assist nursing homes to implement, sustain, and continually enhance an effective, person-centered Resident Council.
 April 10, 2024 11:00
April 10, 2024 11:00Supporting the Neighborhood Enrichment Team (NET) to Enhance the Nursing Home (NH) Experience

Patricia Gagliano, MD
Task Order
1 Lead and Vice
President,
IPRO’s Healthcare Quality Improvement Department

Melanie Ronda, MSN, RN, LTC-CIP, CPHQ
Task 3
Lead,
Infection Preventionist and a Director in IPRO’s Healthcare
Quality Improvement
Department,
IPRO QIN-QIO

Jennifer Wieckowski, MSG
Senior
Executive Director,
Health Services Advisory Group
The NET program enriches the lives of NH residents by recruiting community partners to actively engage in activities that bring value to residents. The NET program evaluates the impact and feasibility of the community taking an active role to improve resident experiences and quality of life.
 April 10, 2024 11:30
April 10, 2024 11:30Using Data to Increase Nursing Home Participation

Nicole Haas, MPH, CPH, CPHQ
Quality Improvement
Initiative Manager,
Alliant Health Solutions

Dee Kaser, RN, CDCES
Quality
Improvement Advisor,
Great Plains

Stephanie Meduna, RN, BSN
Quality
Improvement
Advisor,
Great Plains
Part 1: Since April 2020, Quality Improvement Organizations have received Targeted Response Quality Improvement Initiative (TRQII) referrals from CMS for nursing homes identified as needing assistance with infection control, COVID hot spots, and low vaccination rates. Great Plains QIN operationalizes a multi-faceted best practice approach to facilitate engagement and action leveraging all encounters with nursing homes to improve infection control practices and vaccination uptake.
Part 2: This session will focus on applying high reliability concepts to team members and throughout quality projects to increase nursing home participation in targeted response quality improvement initiatives."
 April 10, 2024 13:00
April 10, 2024 13:00The Quality Improvement Journey: Recertification of Laguna Honda Hospital and Rehabilitation Center (LHH)

Barb Averyt, MHA
Senior
Executive Director,
Health Services Advisory Group

Troy S. Williams, MSN, RN, CPHQ, CPHRM
Laguna Honda
CMS Recertification Co-Incident Commander,
Chief Quality Officer,
San Francisco Health
Network, San Francisco Department of Public Health

Keith Chartier, DrPH, MPH
Executive Director,
Health Services Advisory Group

Jim Bossemeyer
Acting Director,
Division of
SF/Seattle Survey & Enforcement
Centers for Medicare & Medicaid
Services
This presentation will feature insights from the San Francisco Department of Public Health's Chief Quality Officer, HSAG representatives and CMS, offering a comprehensive understanding of the recertification journey of San Francisco's Laguna Honda Hospital and Rehabilitation Center (LHH), the 2nd largest public run skilled nursing facility in the United States. Attendees will gain valuable insights into the strategies employed for successful culture change and sustainability, providing a compelling narrative of resilience, collaboration, and innovation in addressing healthcare challenges.
 April 10, 2024 13:30
April 10, 2024 13:30Innovations In Training and Training Evaluations

Crystal Morse, MS HSA, CSW, CCM
Senior Account
Manager,
Mountain Pacific Quality Health

Laura Myerchin Sklaroff, MA, EdD
Director,
Systemwide Quality Improvement Evaluation,
Comagine Health

Callie Perkins, BSN
Wyoming
Account Manager,
Mountain Pacific Quality Health

Ann Jensen, MPH, CPH
Healthcare
Data Analyst,
Comagine Health
Part 1 – Mountain Pacific Project Firstline team co-created an interactive, team and skills-based activity that provided innovative learning for health care professionals. The Escape Room is a “fun and effective way to learn,” while improving the team culture. Part 2 - Comagine Health QIN-QIO designed and implemented a two-part model to evaluate participant and facility level learning collaborative outcomes over time for single cohorts and across cohorts to access impact and growth. Strategies for learning collaborative evaluation, highlighting an example focused on a Hypertension SMBP learning collaborative will be shared.
 April 10, 2024 14:00
April 10, 2024 14:00Creative Employee Engagement

Tina Sandri, MHSA, LNHA, QCP, RYT-200
Chief
Executive Officer,
Forest Hills of DC
During this unprecedented SNF employee shortage, employee retention is paramount. Forest Hill of DC’s efforts led to a front-page story in the NTY, an AHCA Program of the Year, and the District of Columbia’s first CNA apprenticeship program.
 April 10, 2024 14:30
April 10, 2024 14:30Fireside Chat with CMS Division of Nursing Home

Colleen Frey
Director,
Division of Community
and Population Health,
Centers for Medicare & Medicaid
Services

Eimee Casal, BSN, RN, LNHA
Quality and Safety
Branch Manager,
Division of Nursing Home,
Centers for Medicare &
Medicaid
Services
Shequila Purnell-Saunders
Director,
Division
for Chronic and Post Acute Care,
Centers for Medicare & Medicaid
Services
Eimee Casal, Division of Nursing Homes, Colleen Frey, Division of Community and Population Health, and Shequila Purnell-Saunders, Division of Chronic and Post Acute Care of the Center for Clinical Standards and Quality at the Centers for Medicare and Medicaid Services will discuss several recent and forthcoming initiatives impacting nursing home providers, residents, and families."
 April 10, 2024 15:00
April 10, 2024 15:00Closing Remarks

Jean Moody-Williams, RN, MPP
Deputy Director,
Center for Clinical Standards and Quality,
Centers for Medicare &
Medicaid Services
Posters
Director’s Corner
Recordings